I discuss my treatment algorithm for extended condylectomy defects, focusing on when to use a fibula flap versus a TMJ prosthesis.
I cover important factors in patient selection and highlight situations where a TMJ prosthesis may not be the ideal option.
In this video lecture, we will explore part four of the segmental mandibulectomy treatment algorithm, focusing on various surgical techniques and emerging hardware options that are transforming how I address extended condylectomy defects resulting from cancer resection and trauma cases.
Condylectomy defects present unique challenges for reconstructive surgeons. Given the complexity and variability of these defects, a systematic approach is critical for effective management. In this presentation, I will introduce my traditional repair method for extended condylectomy, which involves using a fibula free flap and a reconstruction plate.
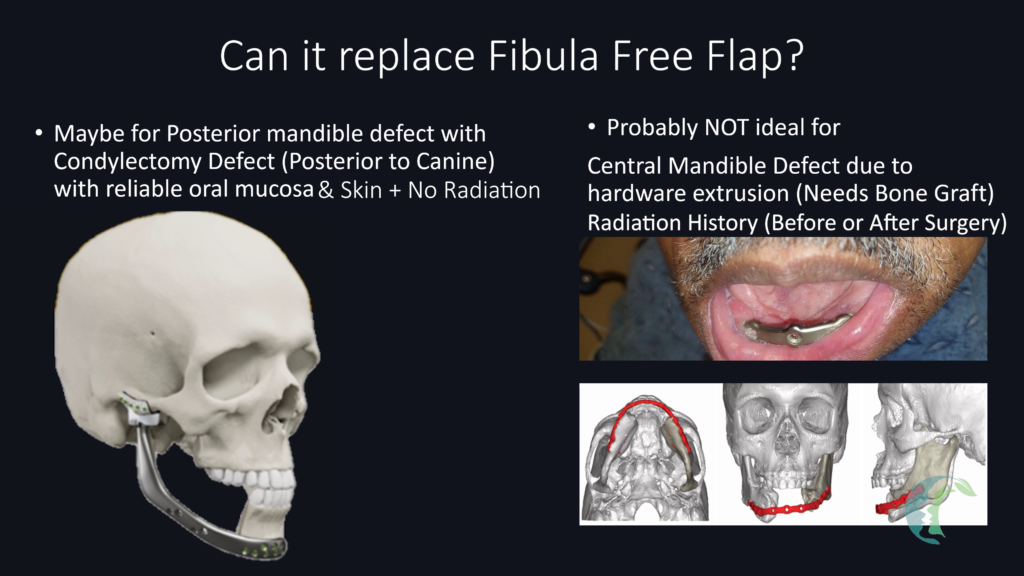
Recent advancements in hardware are reshaping our approach to managing condylectomy defects. One notable innovation is the Stryker TMJ Concepts, which allow for TMJ reconstruction using patient-specific hardware without the need for a free fibula flap in select patients. We will examine this revolutionary hardware and its implications in detail.
The extent of the bony defect and the patient’s medical history—especially prior radiation therapy or postoperative radiation needs—will greatly influences the surgical treatment selection.
For patients requiring postoperative radiation therapy or who have previously undergone radiation, I typically prefer using vascularized fibula free flaps, especially for larger condylectomy defects. If the defect extends to include the anterior arch (medial to first premolar tooth involving the parasymphysis or symphysis), a fibula free flap is the preferred method to avoid delayed hardware or bone exposure involving the anterior mandible segment.
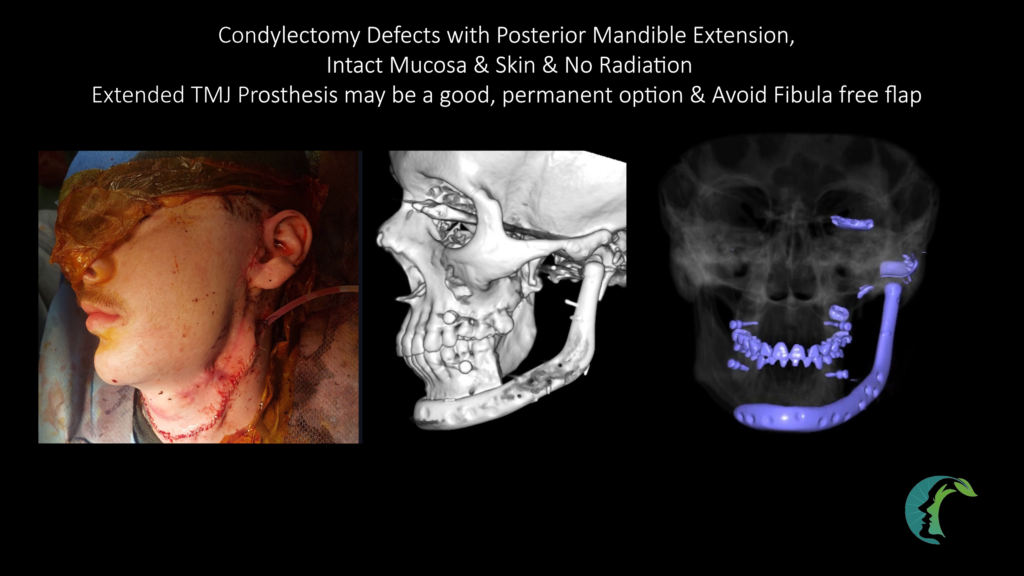
For traumatic injuries resulting in condylar defects, where there is no significant history of radiation, permanent TMJ prostheses, such as Stryker TMJ Concepts, can be considered for smaller defects. In my treatment algorithm, these prostheses are typically reserved for posterior mandible defects (posterior to first premolar tooth/mental foramen and not involving the anterior mandible).
In cases where the patient is considered too high risk for extensive reconstruction (due to high anesthesia risk) or willing to accept malocclusion, I may defer condyle reconstruction entirely and leave the patient in temporary elastic maxillomandibular fixation (MMF) to help guide them into improved occlusion with the expectation that they will have varying degree of permanent malocclusion. This may not be an issue in patients who are at baseline edentulous. 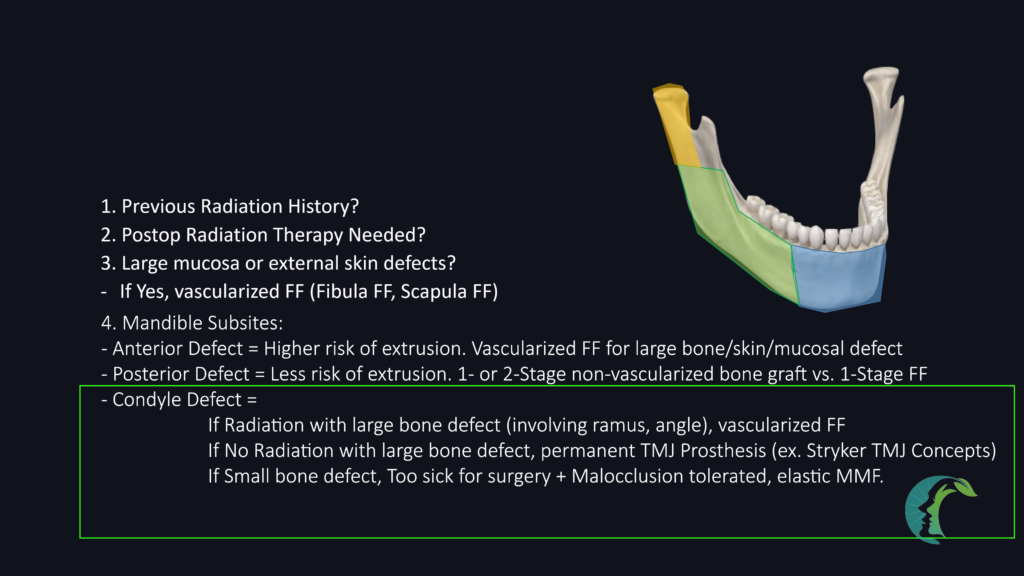
Consider a patient with retromolar trigone squamous cell carcinoma, presenting with a condylectomy defect extending to the posterior body, along with a significant mucosal defect, requiring postoperative radiation therapy. 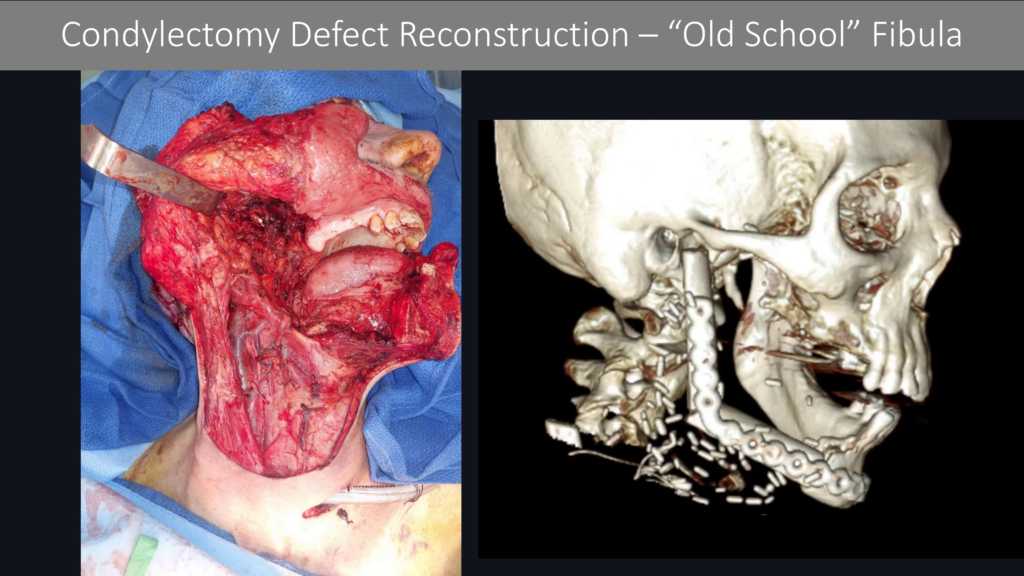
In this case, my preferred reconstruction is a fibula free flap, primarily due to two factors: the need for postoperative radiation therapy and the requirement for immediate mucosal reconstruction due to significant mucosal defect.
Preoperatively, it is essential to evaluate the patient’s CT scan for patient’s with retromolar trigone SCC, particularly in the sagittal plane, to assess for bone resection margin. 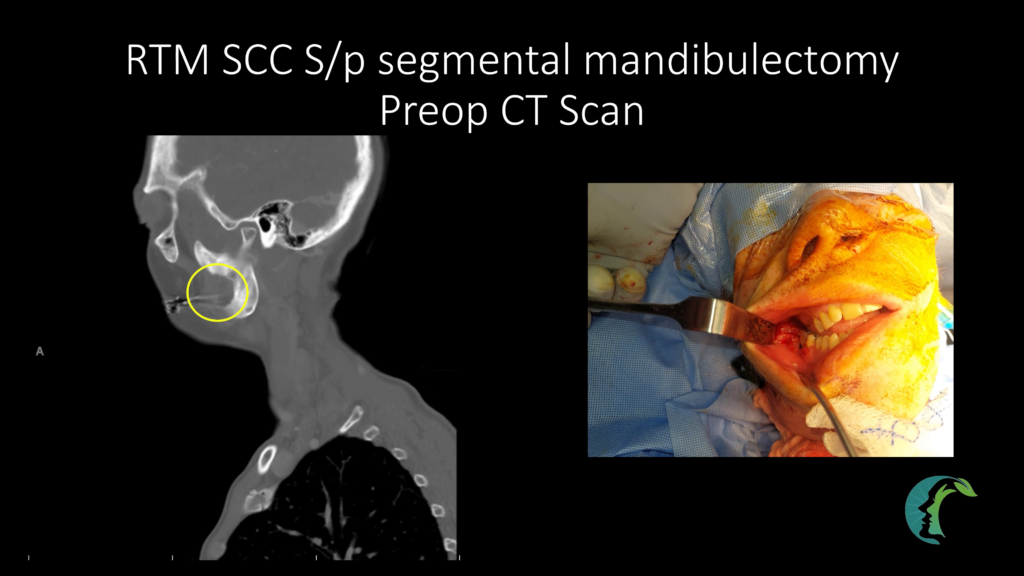

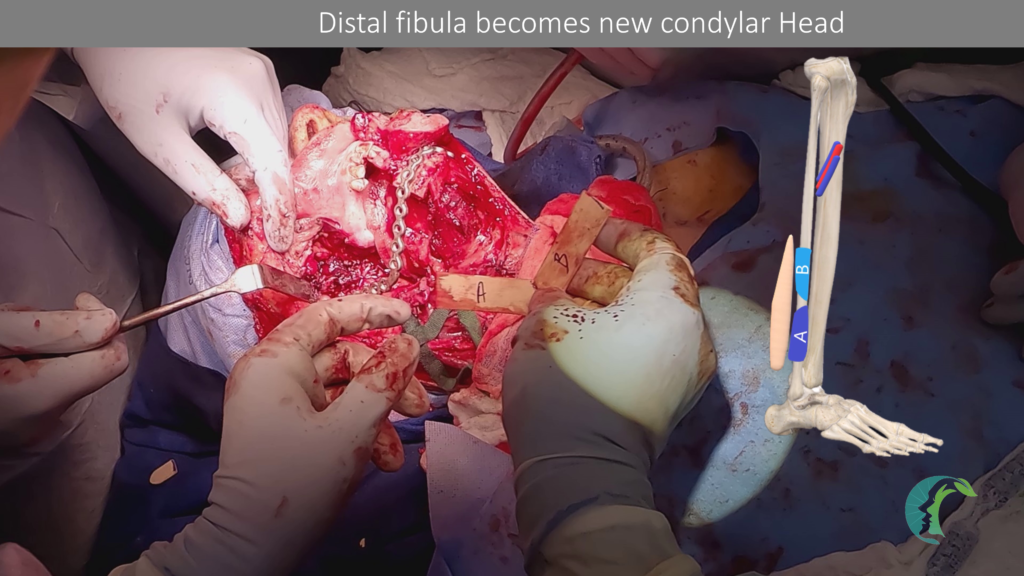
In this particular patient, the remaining condyle segment is too short to accept three screws for a standard reconstruction plate. If there is inadequate room for screw placement, it is preferable to remove the entire condyle and replace it with the distal fibula as in this particular patient.

Preoperative virtual surgical planning can facilitate the design of custom hardware, particularly in cases involving angle-to-angle defects, extended condylectomy defects, or when pathological fractures obscure normal bony landmarks and premorbid occlusion.
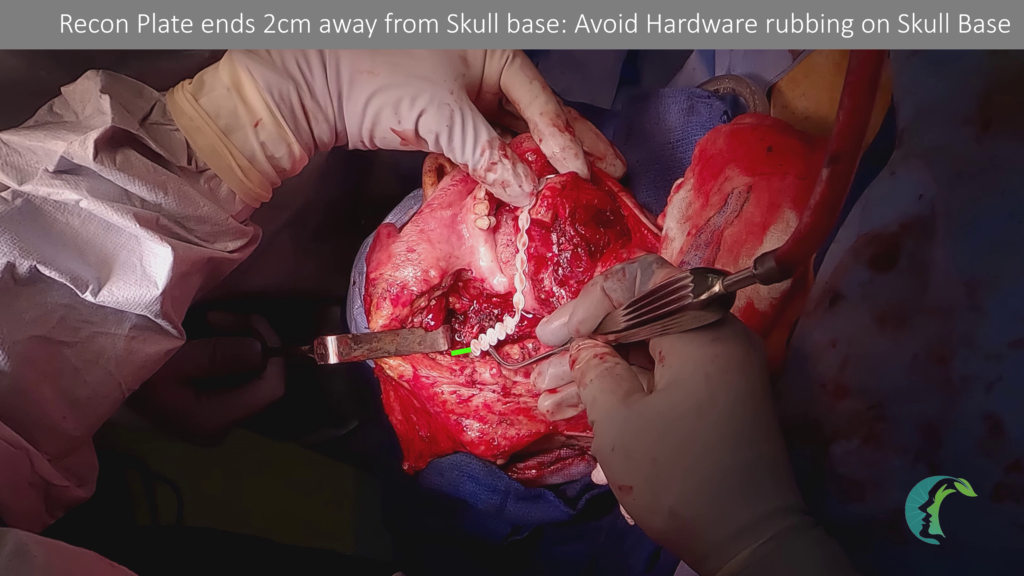
Alternatively, you can manually bend a reconstruction plate using a sterile tongue blade as a fibula-cutting template. The distal fibula serves as the new condyle, while the proximal segment recreates the angle/posterior body segment. Once the fibula bone is fixated, the skin flap is secured to reconstruct the mucosal defect.
To prevent hardware exposure after radiation therapy, it is essential to deepithelialize the remaining skin flap and drape it over the fibula and reconstruction plate. This step is crucial for safeguarding the reconstruction from delayed exposure, particularly in high-risk cases (radiation therapy, chronic malnourishment, chronic infection, poor tissue quality).
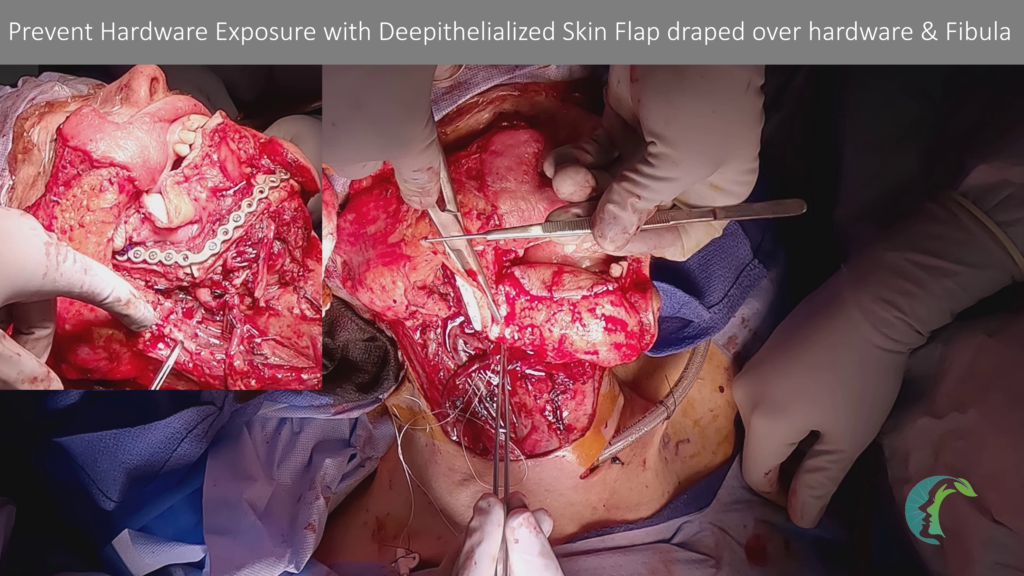
When closing the neck, the priority is to avoid compressing the free flap vessels, rather than replicating the original skin closure. Using towel clamps, start approximating the skin flap from the side where the free flap vessels are located, and recruit skin from the opposite neck side to minimize tension over the flap vessels. 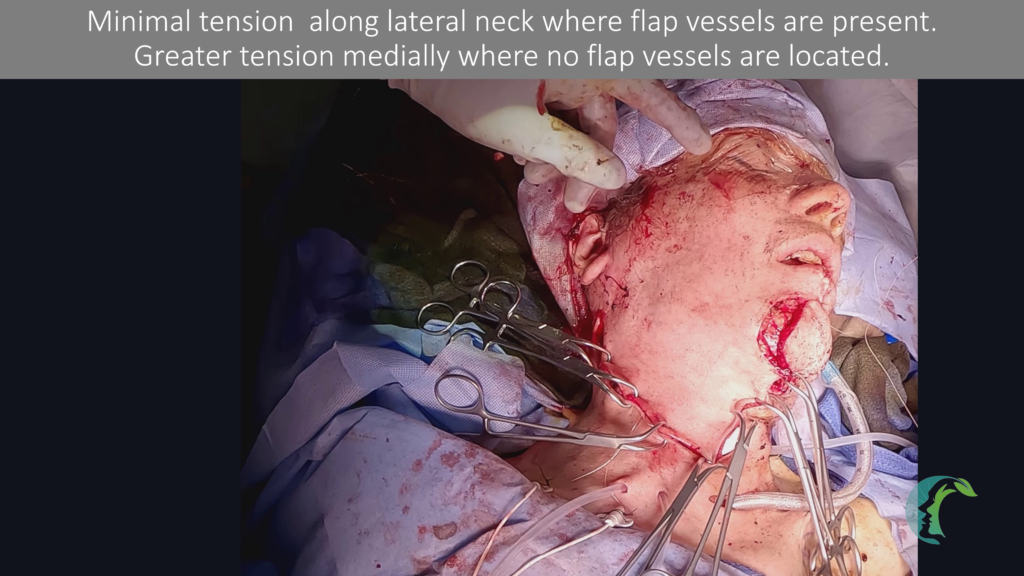
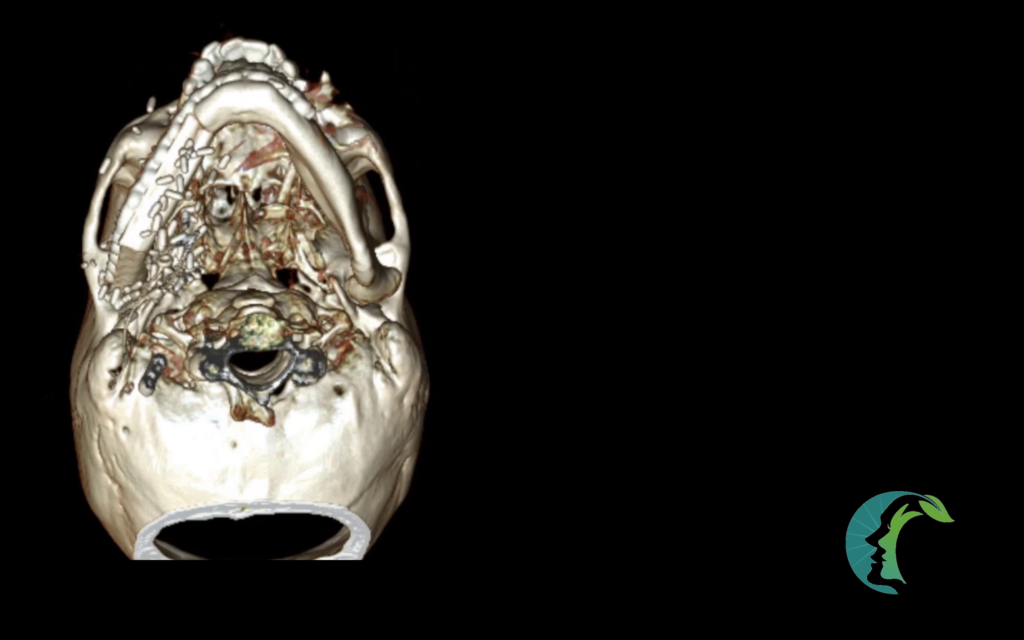
I routinely obtain postoperative CT scans to assess hardware alignment. From the frontal view, the newly reconstructed fibula should have good vertical height symmetry with the opposite condyle. From the basal view, the mandibular contour should mirror the remaining native mandible, forming a trapezoid shape. 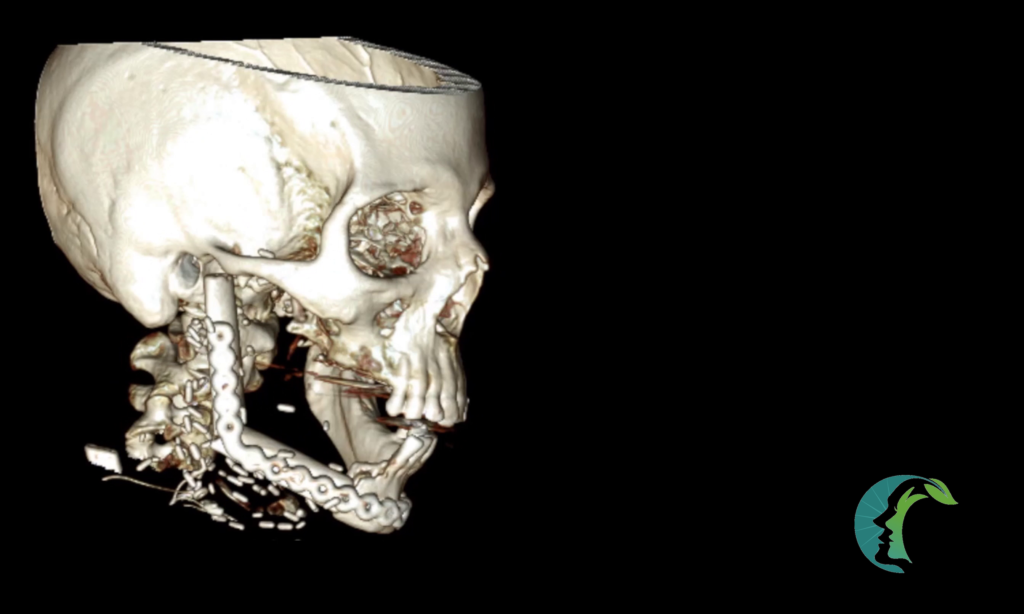
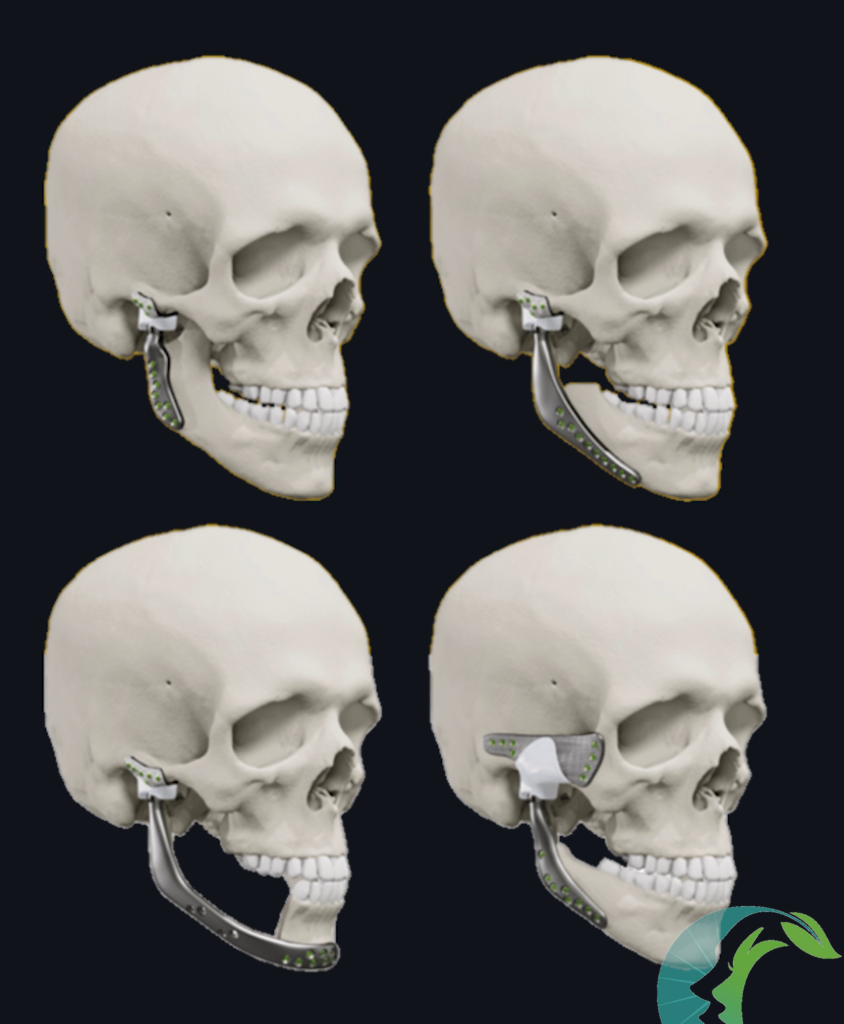
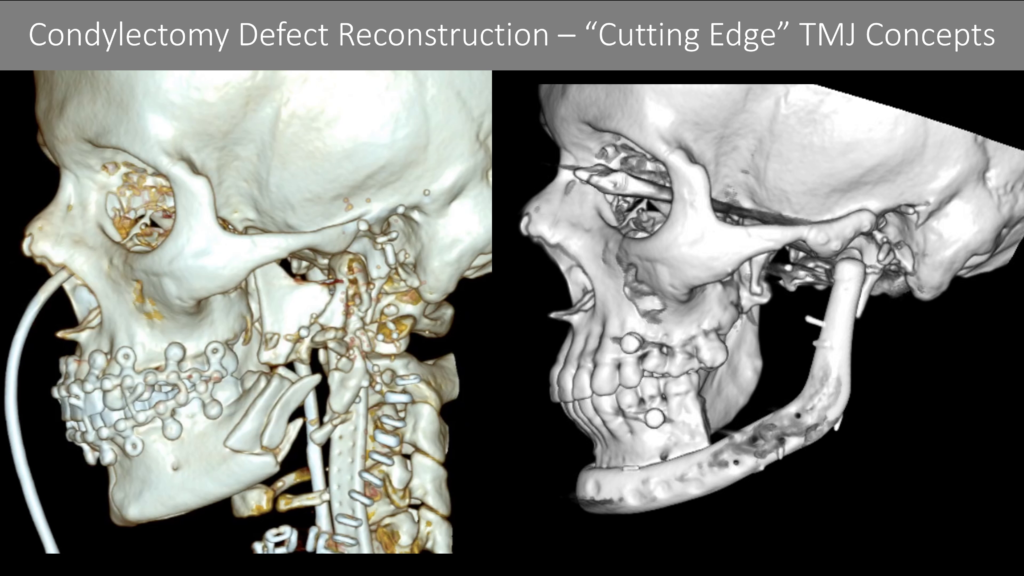
Permanent TMJ prostheses, such as Stryker TMJ Concepts, are gaining wider recognition. There are multiple variations of the hardware, ranging from isolated condylar defects to defects involving the posterior mandibular body and zygomatic arch.
A pivotal study by Wolford et al. reviewed outcomes from 111 patients over 20 years, reporting no hardware failures and significant quality-of-life improvements for patients with TMJ prosthesis.
Permanent TMJ prostheses may be a suitable option for patients who meet the following criteria:
It is essential to recognize the limitations of permanent TMJ prostheses, particularly in the following cases:
In such cases, a traditional approach of using fibula free flap may result in more reliable reconstruction with lasting structural integrity.
To contextualize the use of this technology, let’s examine a case involving a gunshot-related trauma that resulted in an extensive surgical defect at the mandibular angle and condyle. The patient had a relatively small mucosal defect amenable to primary closure, with no history of radiation therapy, which allowed for a two-stage reconstruction using TMJ Concepts hardware, without the need for a free fibula flap.
The CT scan of this patient revealed the severely comminuted mandibular angle and condyle, underscoring the need for careful planning and a tailored intervention strategy.
Intraoperatively, additional problems were discovered that required surgical correction. The surgical issues identified were:
In a complex case with multiple surgical issues, I try to prioritize and figure out surgical intervention unique to each of them to help me figure out how to stage out procedures when necessary.
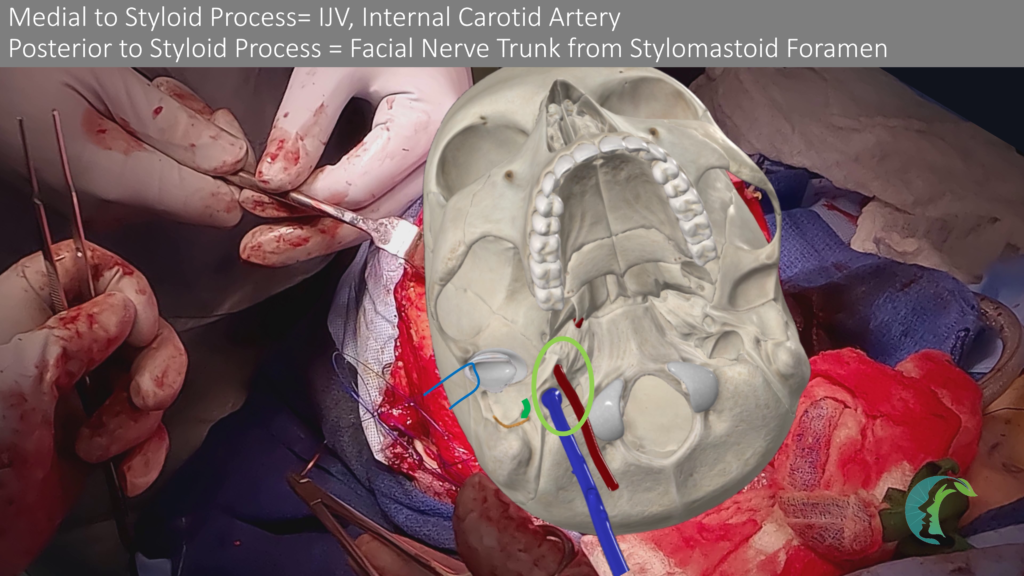
The initial focus must be on addressing the intraoral mucosal defects as failure can lead to necrotizing neck fasciitis and sepsis. Following this, the transected external auditory canal should also be repaired before considering the placement of any mandible hardware near the TMJ region as any leakage from the external auditory canal could lead to significant hardware infection. Third, since this mandibular fracture resulted from a gunshot injury, there is a high degree of delayed osteomyelitis and hardware infection. As such, aggressive debridement of bone is warranted to until healthy bleeding bone is encountered with careful selection of mandible hardware. As noted from my other lecture, comminuted mandible fractures from high projectile injury is treated very differently from blunt trauma especially if there is massive mucosal or skin defects also present. Please see this lecture for further information. Next, the facial nerve continuity should be restored. Finally, definitive condyle reconstruction will be planned for a staged surgery, while temporary TMJ hardware is placed during the initial procedure.
In this case, the mucosal laceration near the retromolar trigone was closed primarily and reinforced with soft tissue along its undersurface, creating a two-layer closure over the mandible reconstruction plate.
Similarly, the external auditory canal (EAC) injury was repaired with a canalplasty, carefully closing the remaining cartilage and reinforcing it with a superiorly based sternocleidomastoid muscle flap. If the EAC repair had been unreliable, I would have deferred placing the temporary TMJ prosthesis, as it could lead to hardware extrusion into the injured EAC or hardware infection from EAC leakage onto the prosthesis.
For significant nerve gaps, a cable graft may be necessary to restore facial nerve continuity while avoiding tension that could compromise blood perfusion to distal nerve ends. 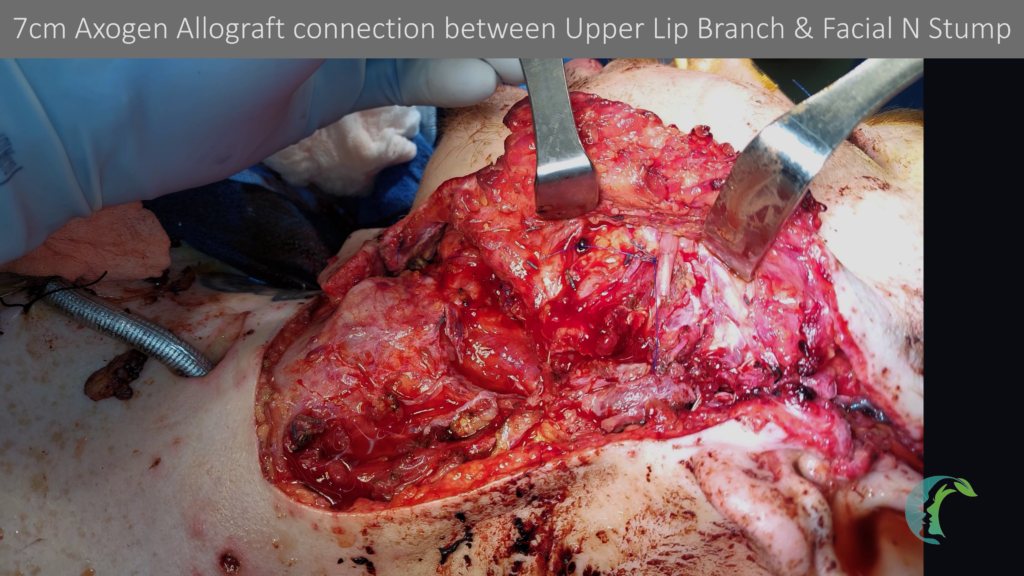
For additional information, you can review my facial nerve reconstruction lecture.
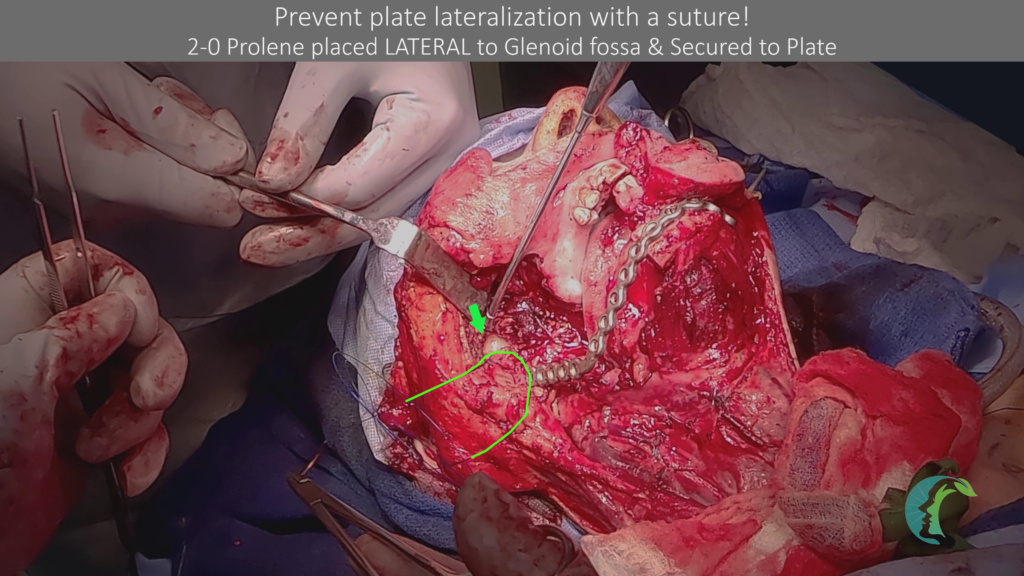
In this patient, we decided to use Stryker TMJ Concepts for the condyle defect. As such, we placed a temporary TMJ prosthesis with a reconstruction plate to help with the second surgery soft tissue dissection. 
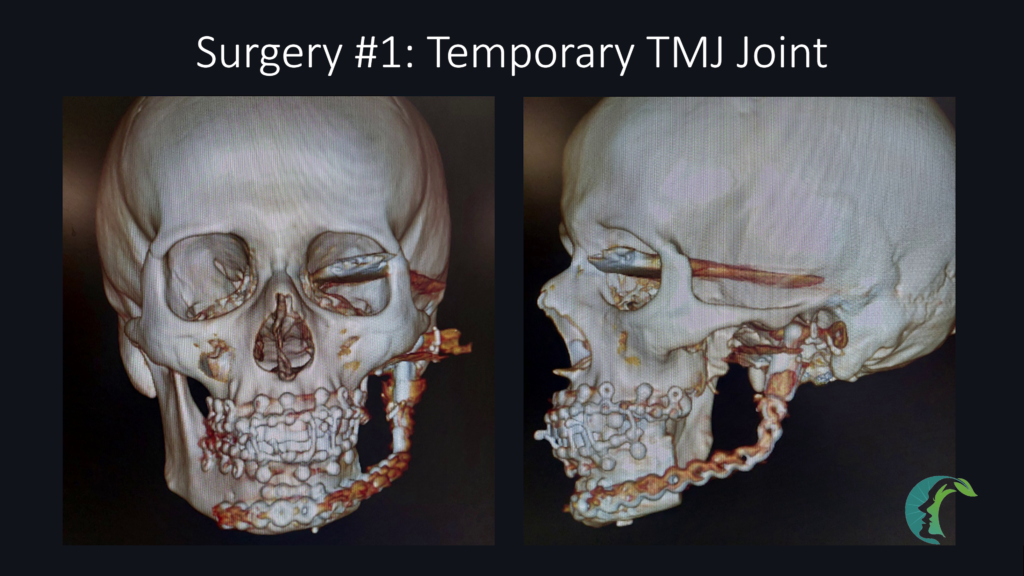
In the second surgery that was performed 3 months later, a custom TMJ prosthesis was placed to reconstruct extended condylectomy defect that involved condyle, angle and posterior body without using a fibula free flap. 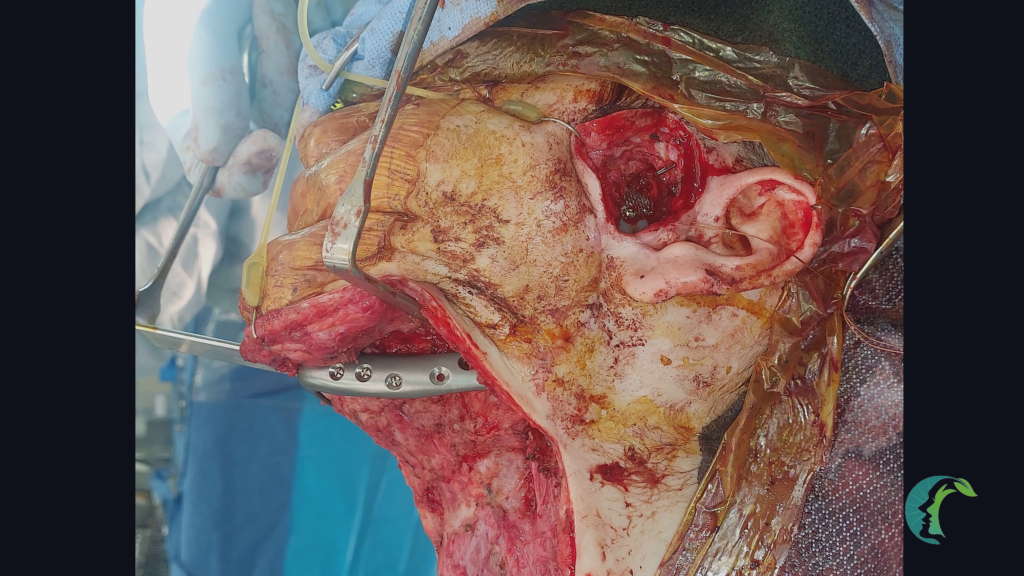
The evolving landscape of surgical innovations for condylectomy defects has dramatically improved patient care possibilities. TMJ reconstruction using permanent prostheses presents an exciting frontier in reconstructive surgery.
It is crucial to carefully screen patients and develop surgical plans that account for individual factors to ensure optimal treatment outcomes. As technology advances, it would benefit clinicians to stay informed and adaptable to continue delivering the highest standard of care.