Key Concepts:
- Perform neck dissection as your attending faculty recommends. Then learn how it is performed in this particular video and incorporate techniques you like into your surgical steps
- A key difference you will see in this video is that I prefer to lift neck dissection content away from internal jugular vein. I prefer this method as I am moving things away from great vessels once they are fully exposed.
- Most head & neck surgeons will perform neck dissection where they sweep neck content towards the great vessels. This is also the way I was trained. I feel more at ease when I have already found the great vessels and is fully dissected. In essence, which way you dissect is a matter of preference but most importantly, you should know how to do neck dissection both ways!
- In advanced cancer involvement (See Oncology 601), you will have to remove the cancer and lymph nodes by lifting the tumor away from the great vessels. In that situation, you will require approach from multiple directions.
- Please watch Fundamentals 201 Lecture before watching this to learn key anatomic relationship.
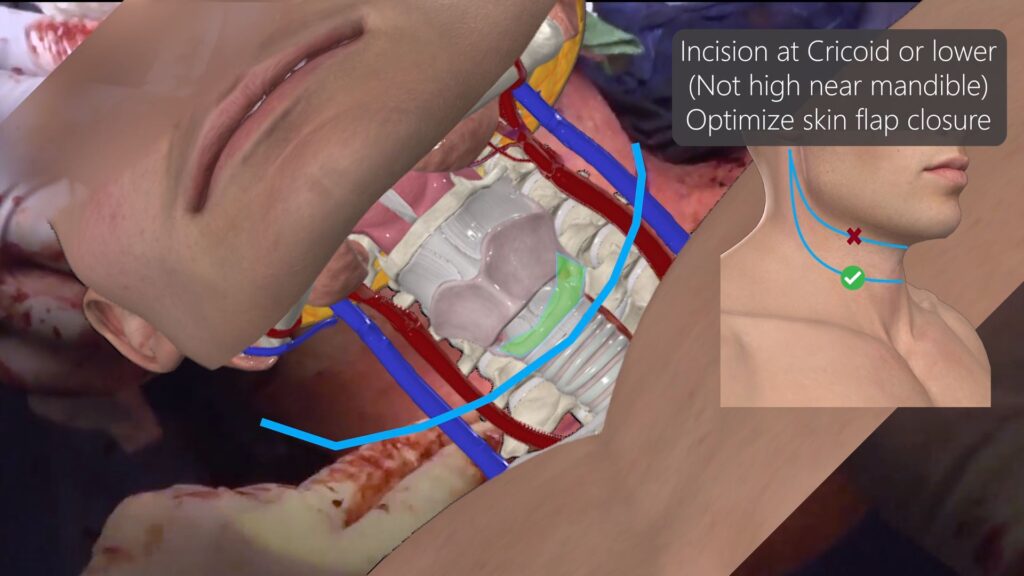
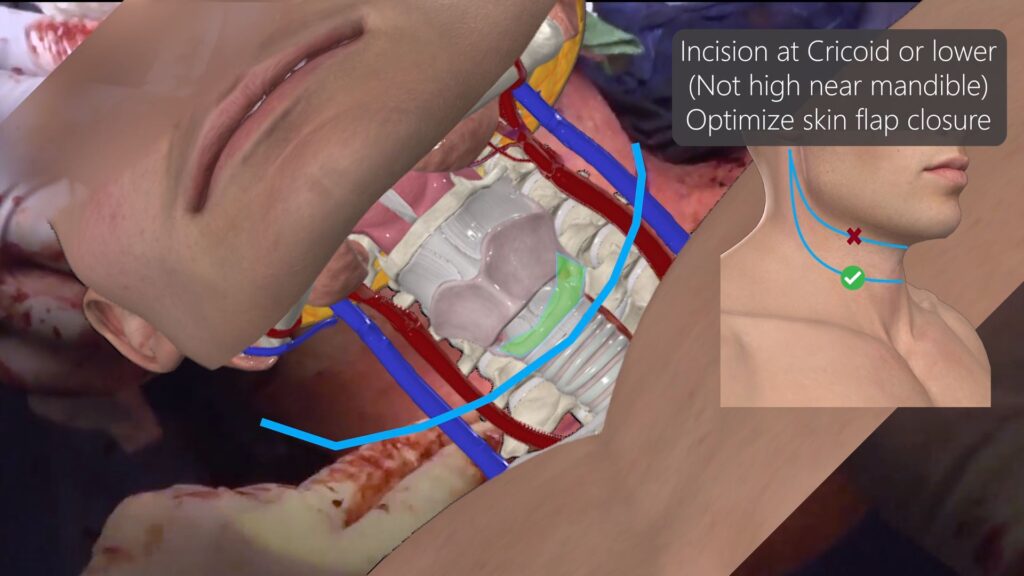
- If performing bilateral neck dissection, design wide apron incision that is placed inferior to cricoid to help with skin closure especially if patient has previous radiation history. If skin flap is designed too high or too narrow, skin closure will be difficult and the skin flap may also die from poor perfusion (in radiated patients).
- In radiated neck patients, once you open the neck, it will most likely not close due to severe contracture. Design your skin flaps avoiding great vessels immediately under the incision if SCM missing.
- Think of neck dissection as different zones. Each levels have key structures that need to be identified & protected. Anticipate structures before you visually see them.
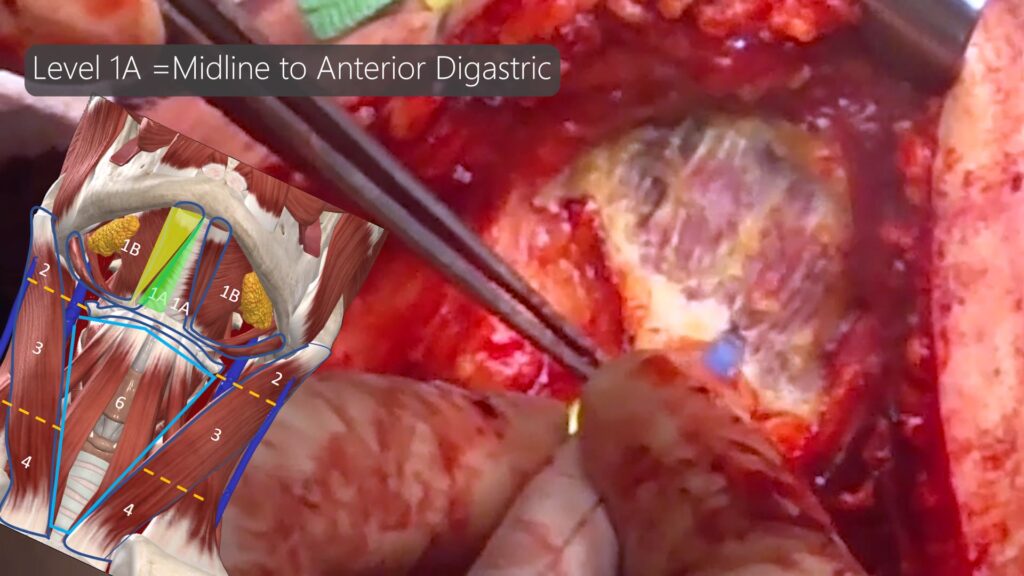
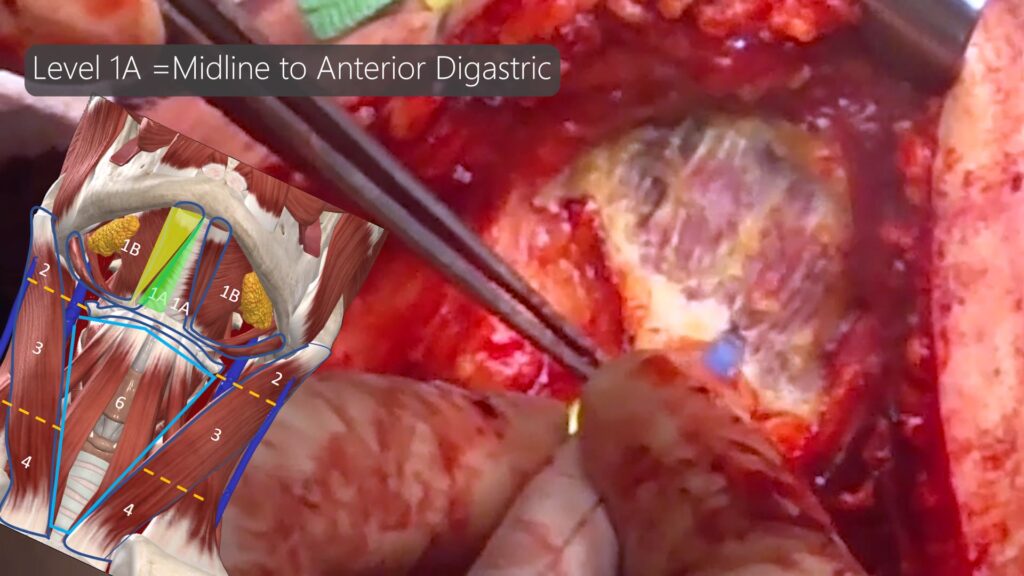
- Level 1A = Midline down to muscular floor above hyoid. Nothing critically important except marginal mandibular nerve along lateral aspect.
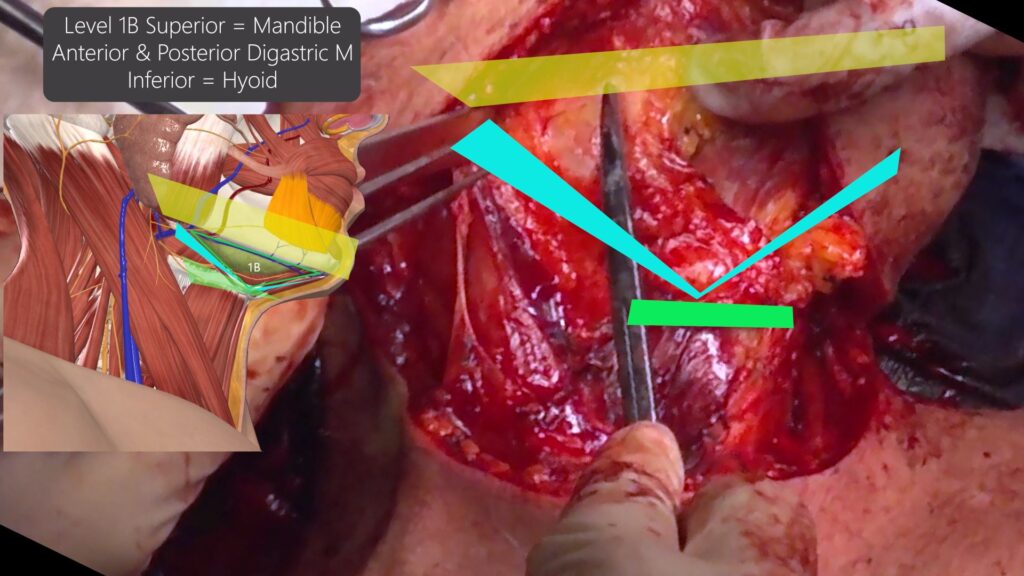
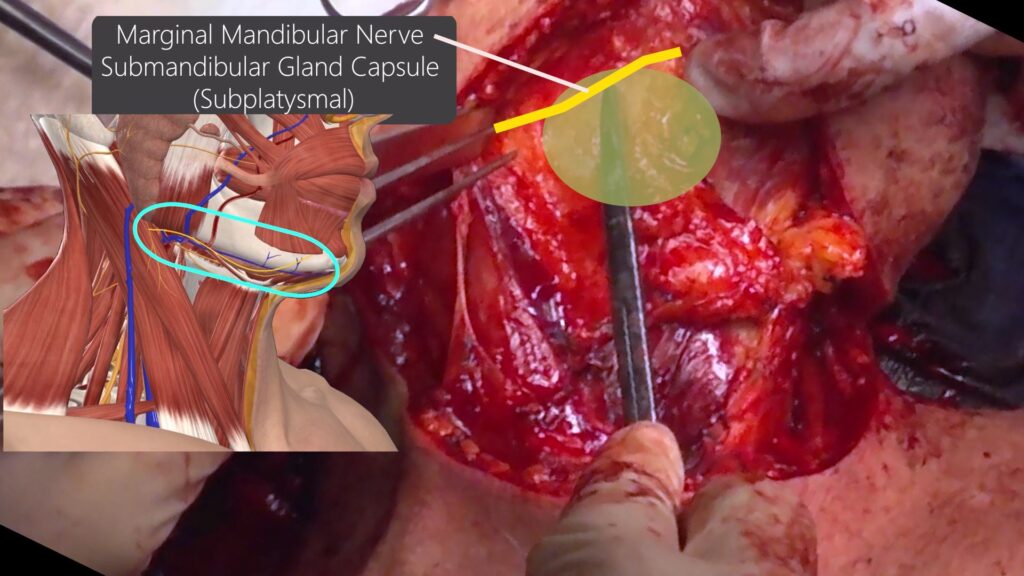
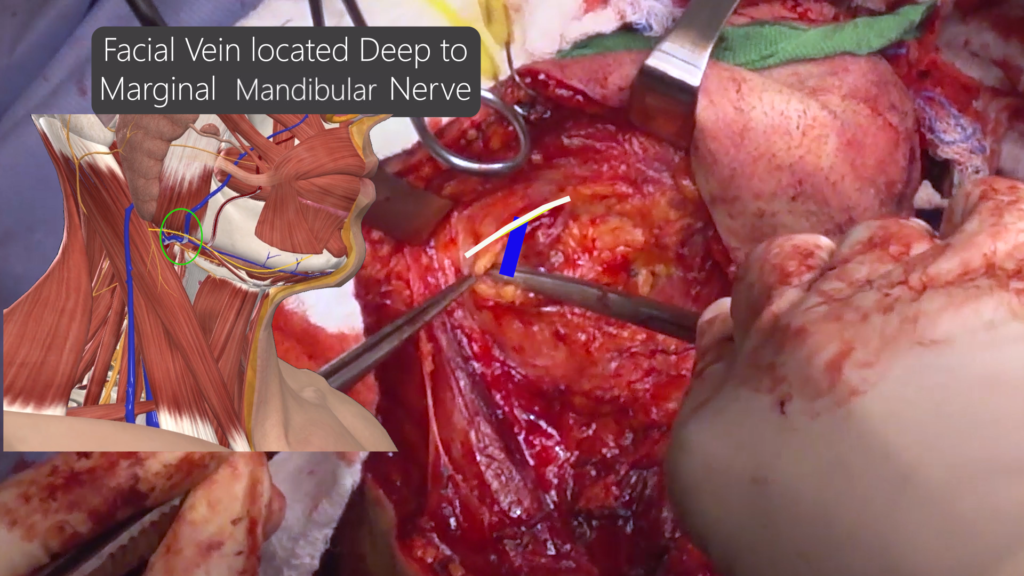
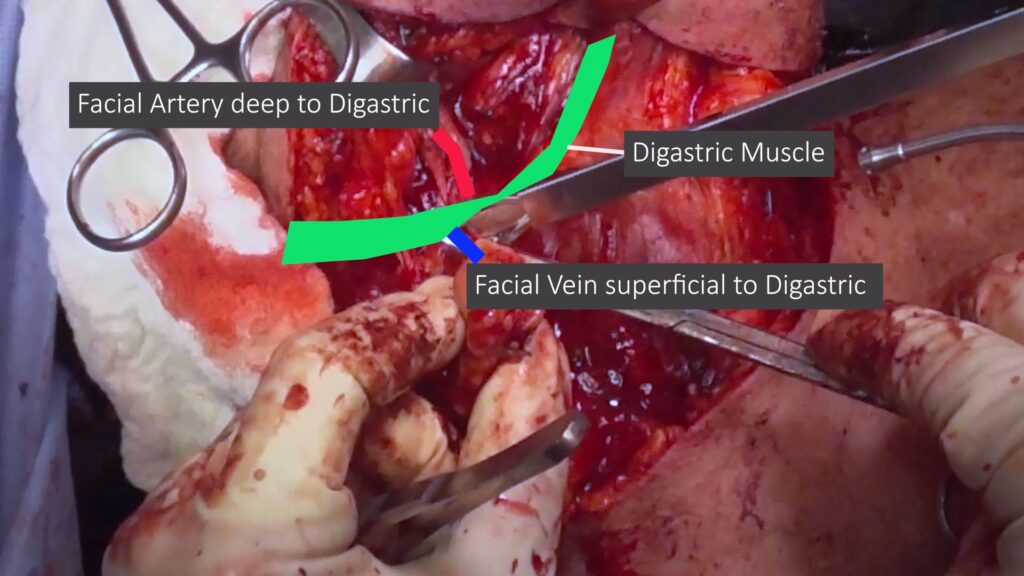
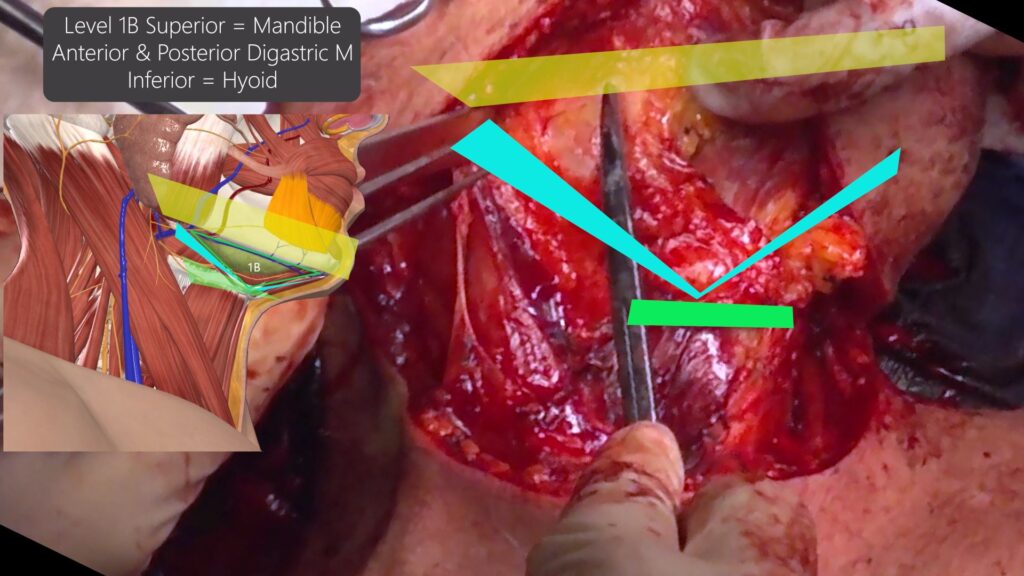
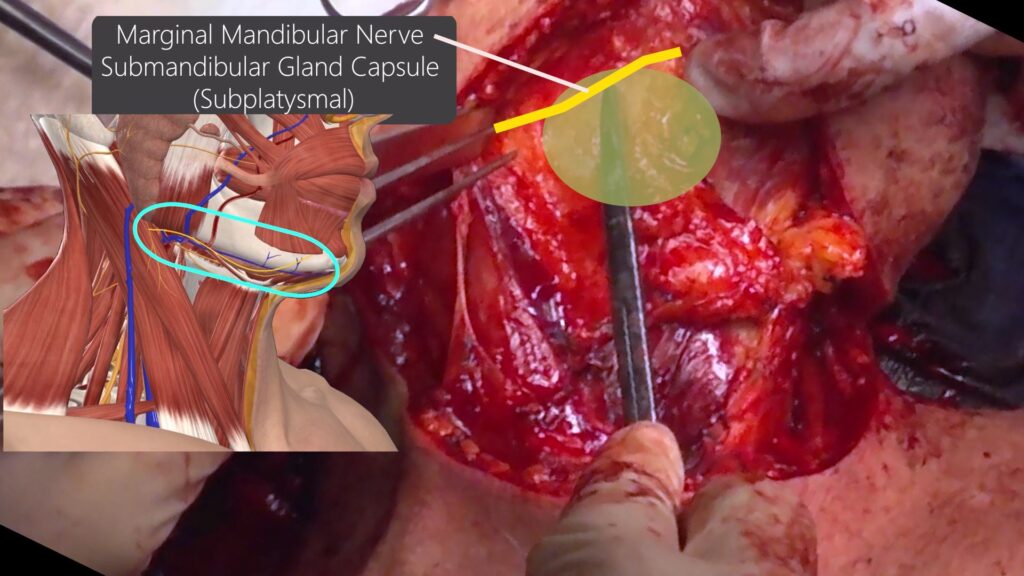
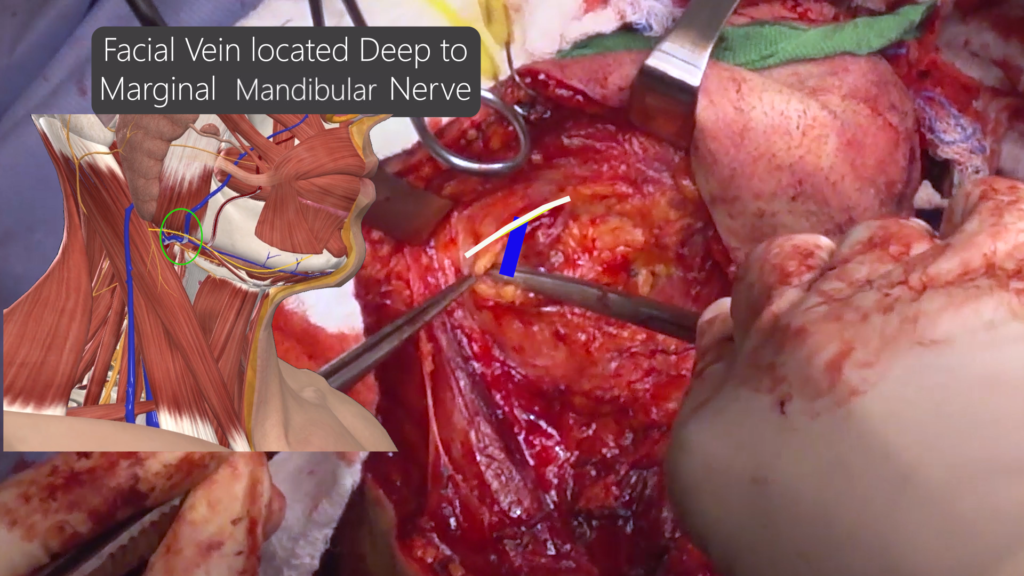
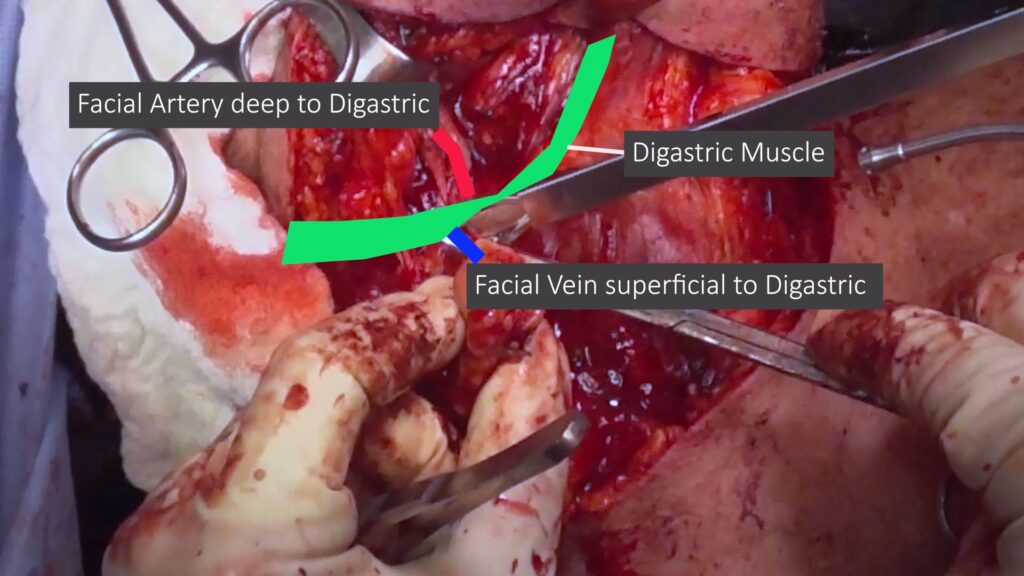
- Level 1B= Marginal mandibular nerve (superficially), Facial artery, facial vein, submandibular gland, mylohyoid, digastric muscle, lingual nerve
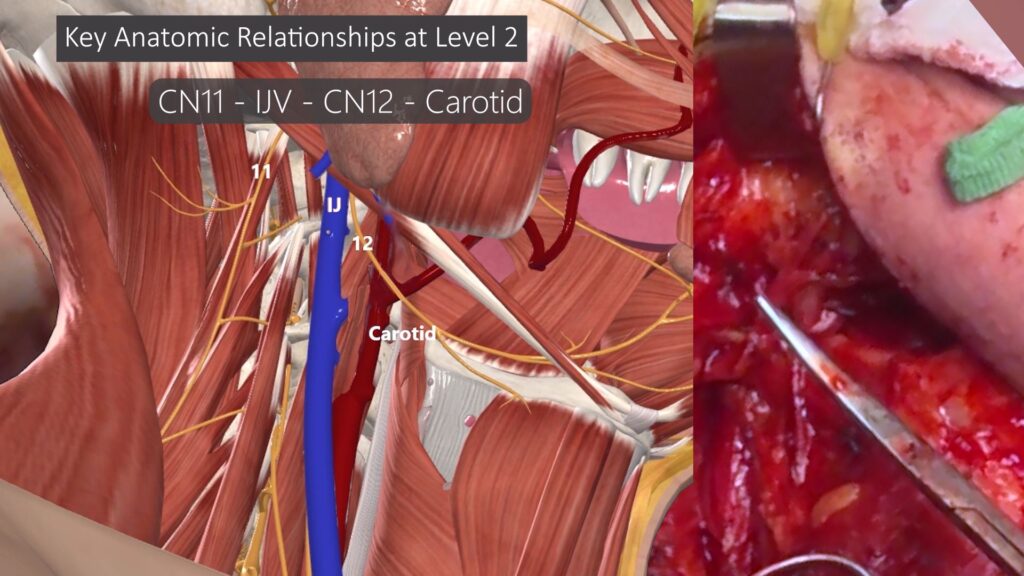
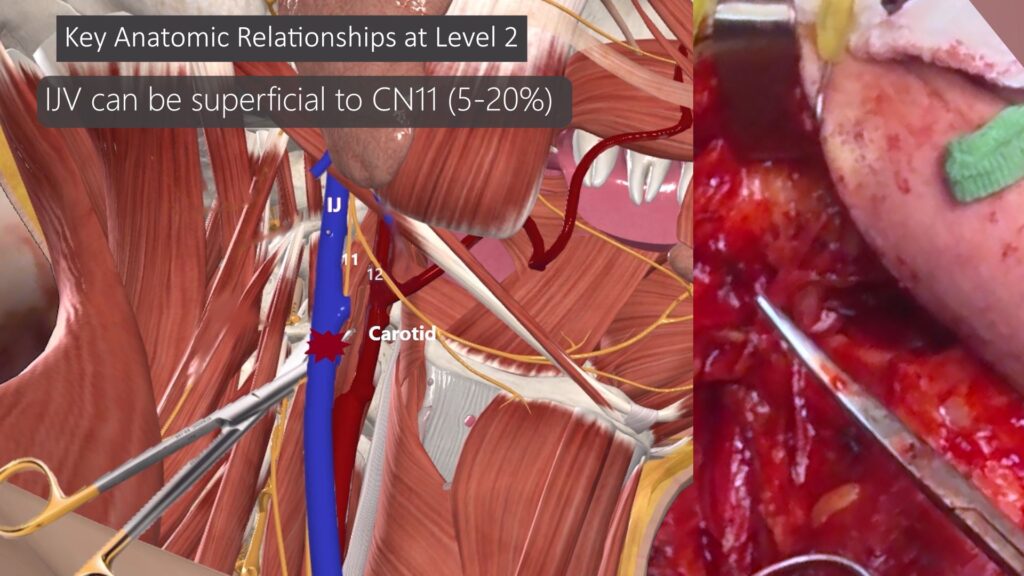
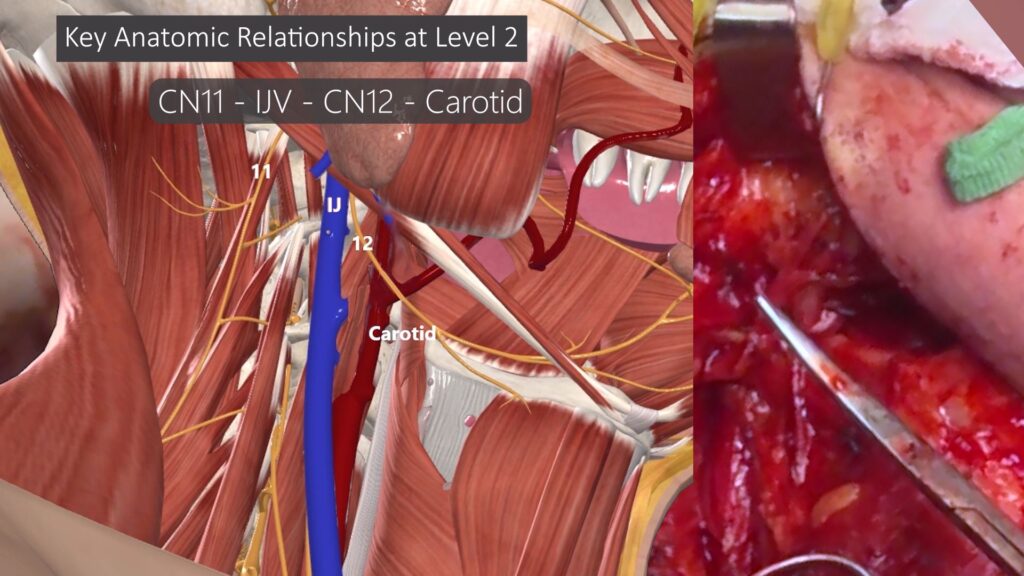
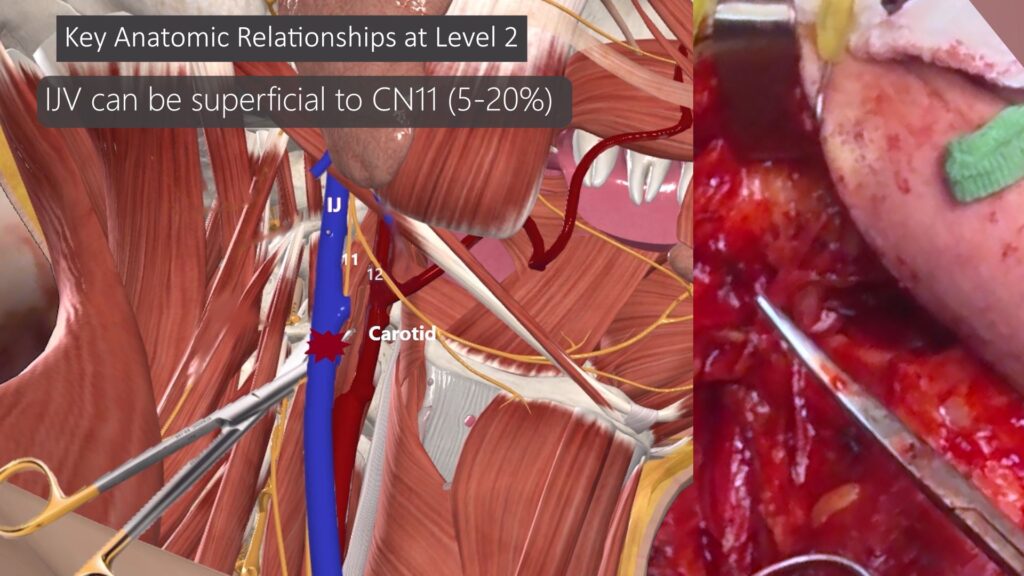
- Level 2 = CN 11, IJ, CN 12, Carotid Artery. Understand key variation to this relationship to avoid cutting through IJV by accident.
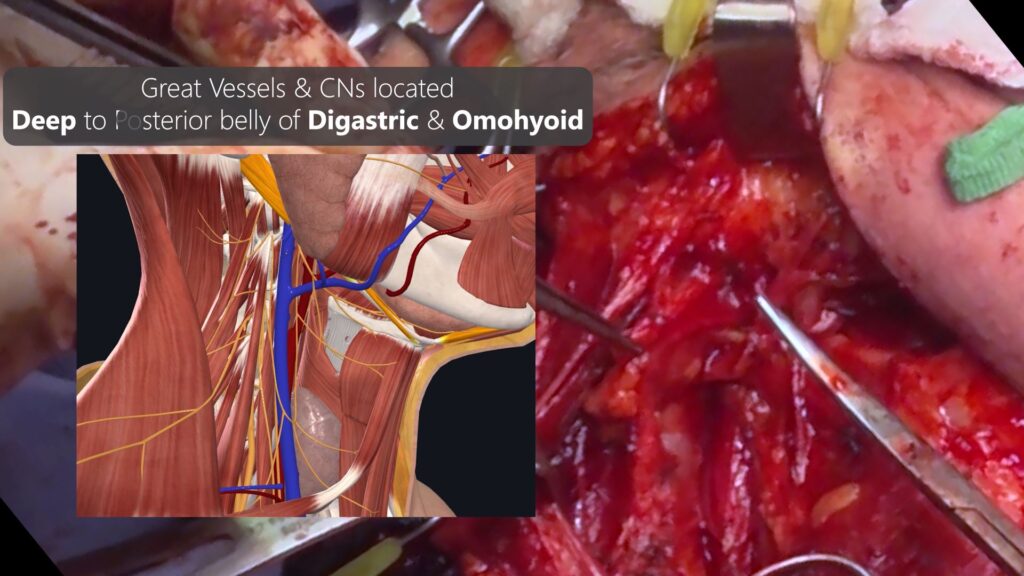
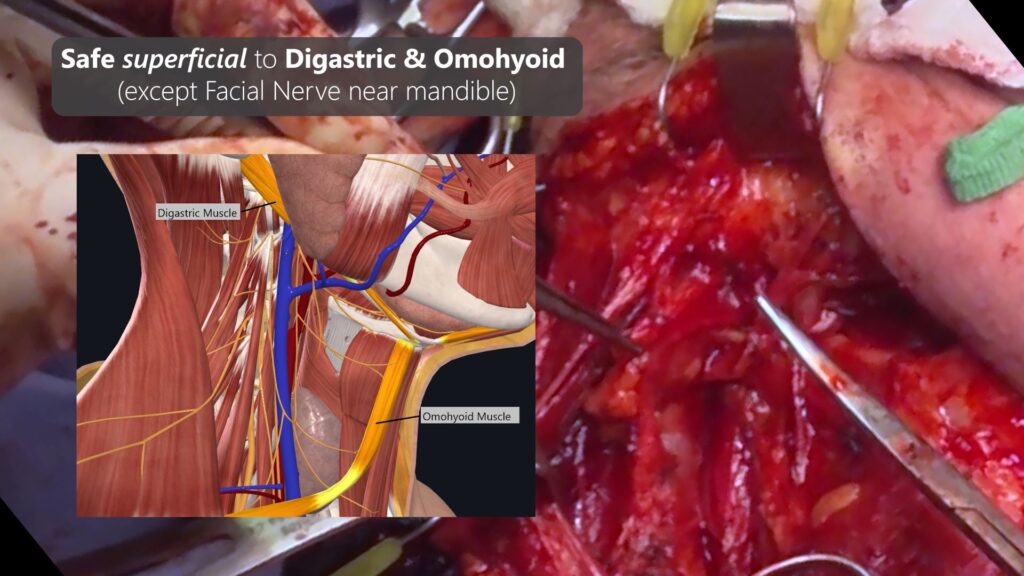
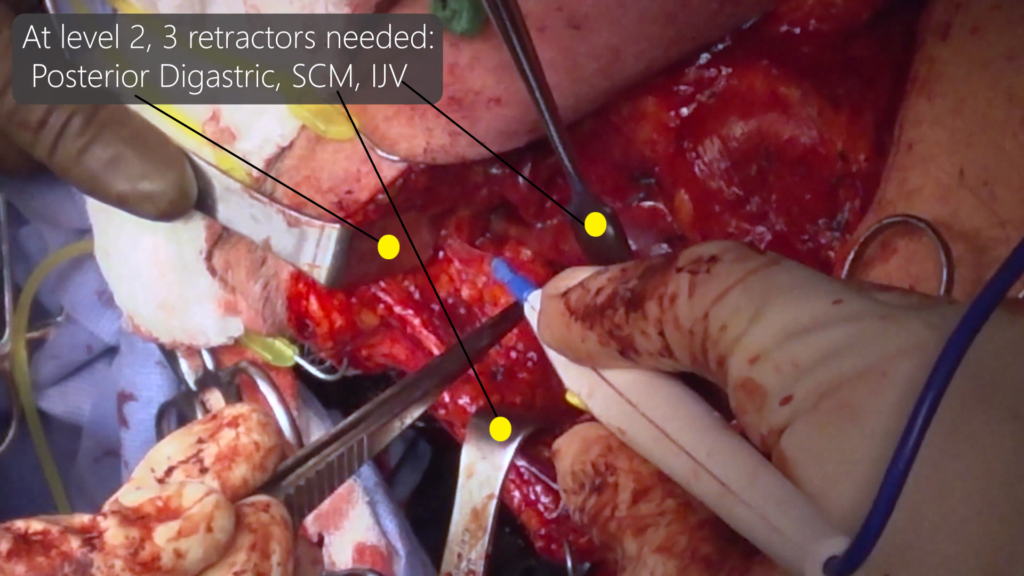
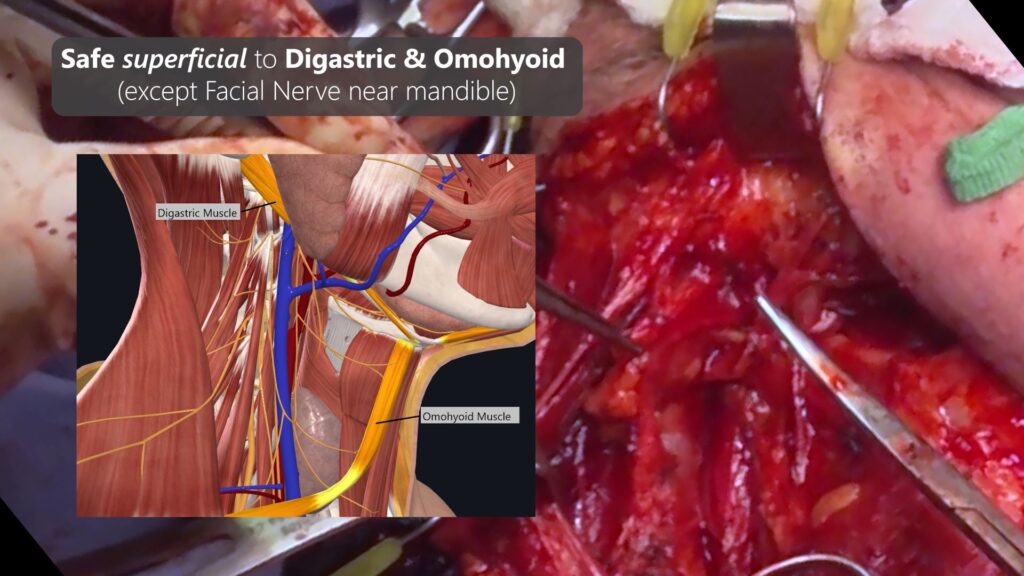
- Great Vessels & Nerves are deep to Digastric & Omohyoid Muscle
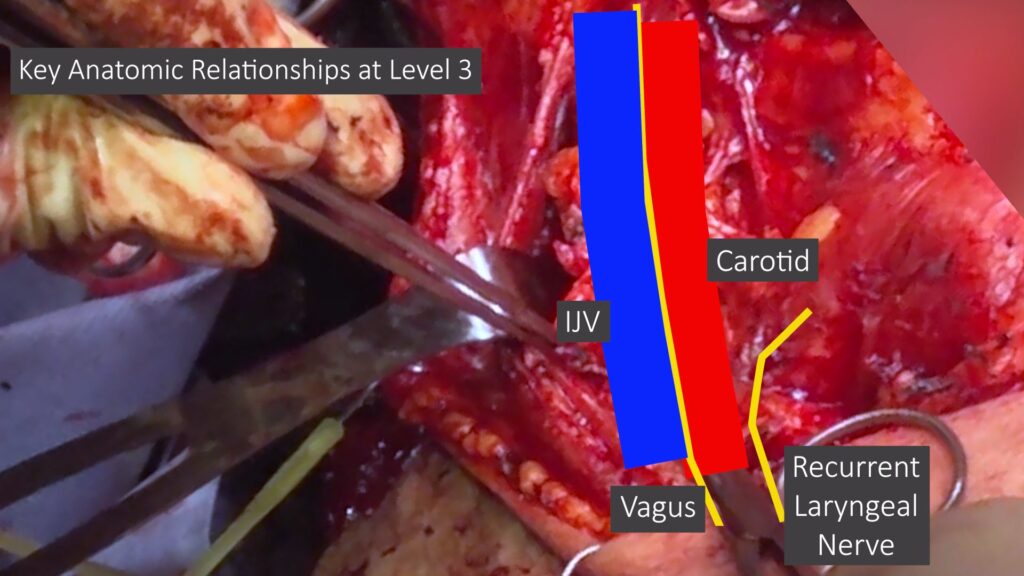
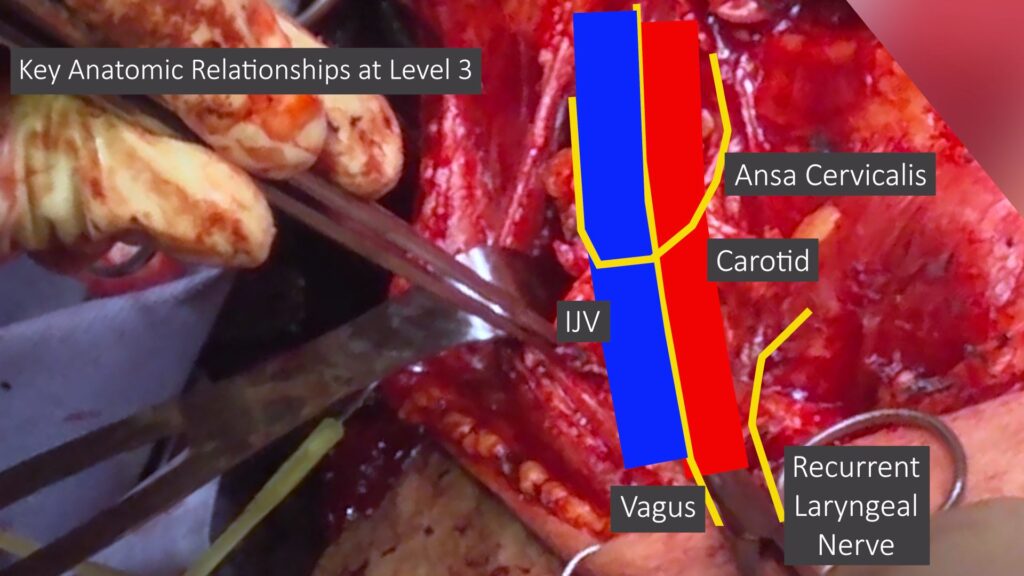
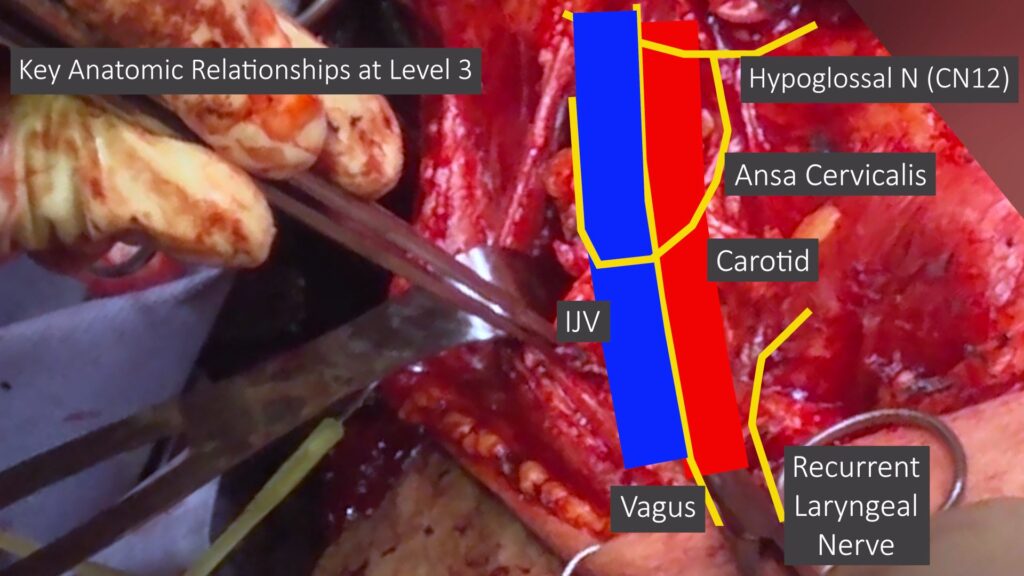
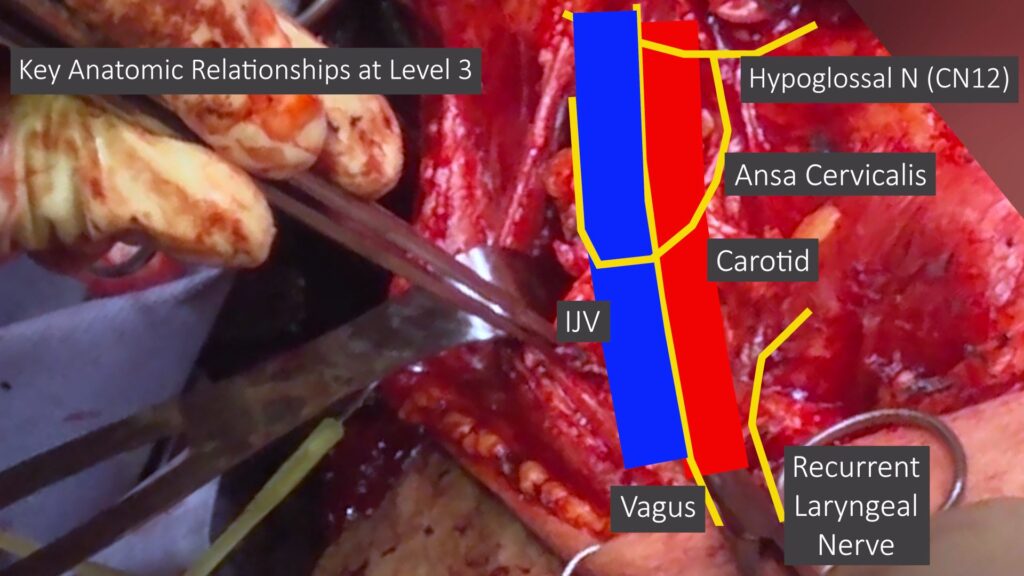
- Level 3 = IJ, Carotid, Vagus Nerve. Easier to identify deep tissue plane at level 3
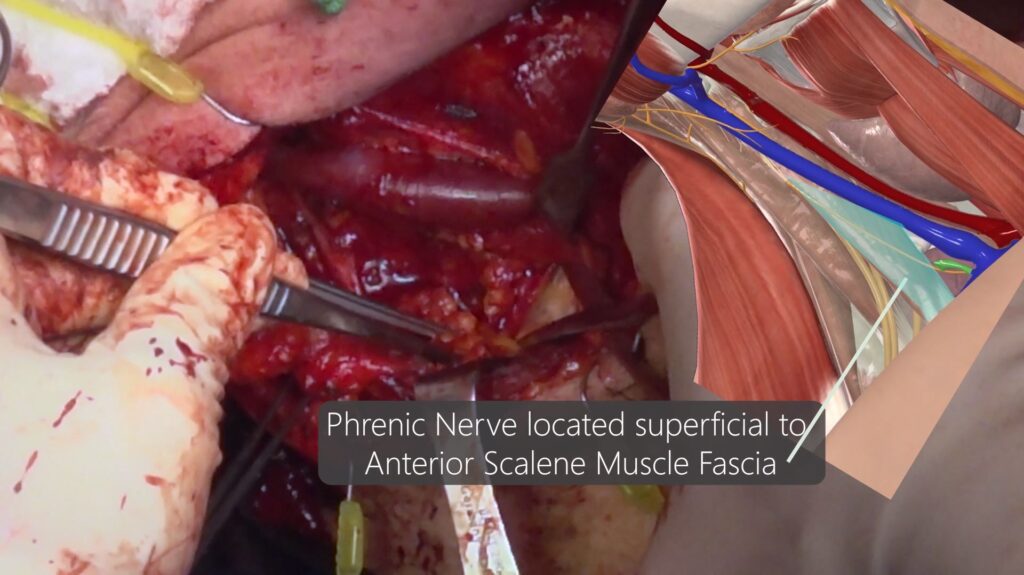
- Level 4 = Transcervical artery/vein, phrenic nerve, brachial plexus, anterior & middle scalene muscles
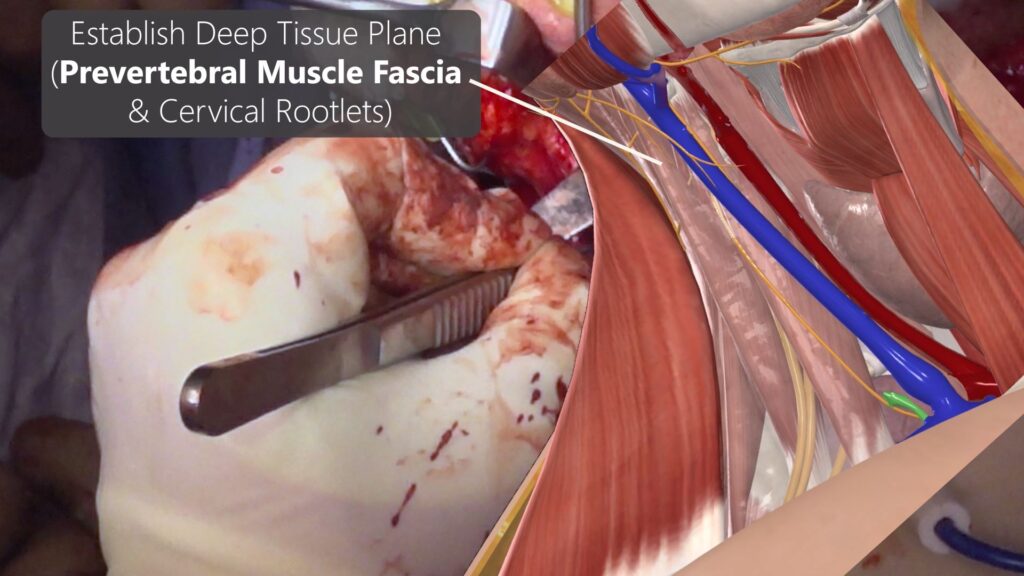
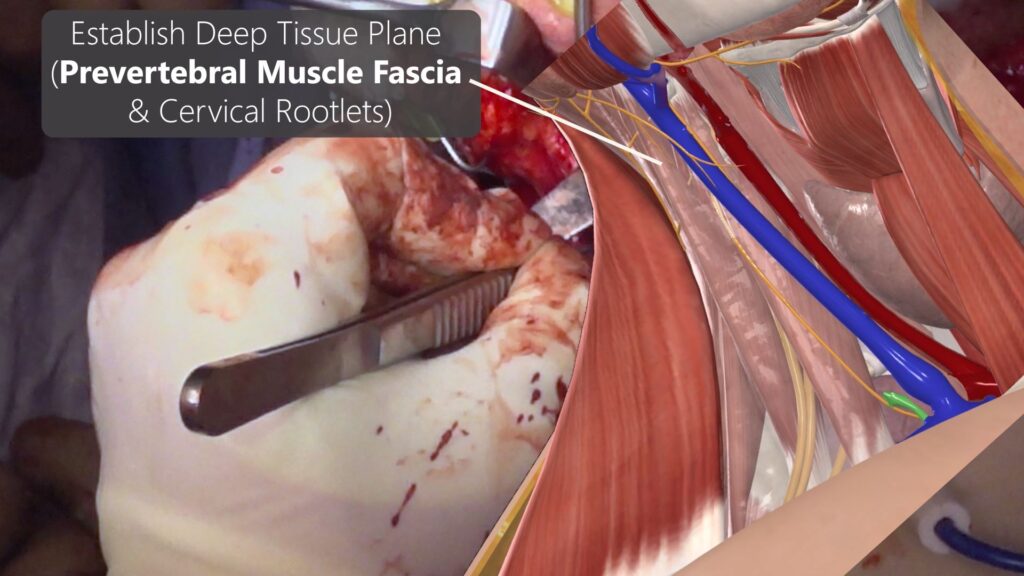
- Deep Plane for Level 2-3 = Prevertebral Fascia, Cervical Roolets
- Deep Plane for Level 4 = Stay superficial to Phrenic Nerve. Phrenic Nerve is located on top of anterior scalene muscle fascia. If you see anterior scalene muscle fibers, you went through the muscle fascia and is TOO DEEP! Avoid phrenic nerve injury.
Neck Skin Incision Design

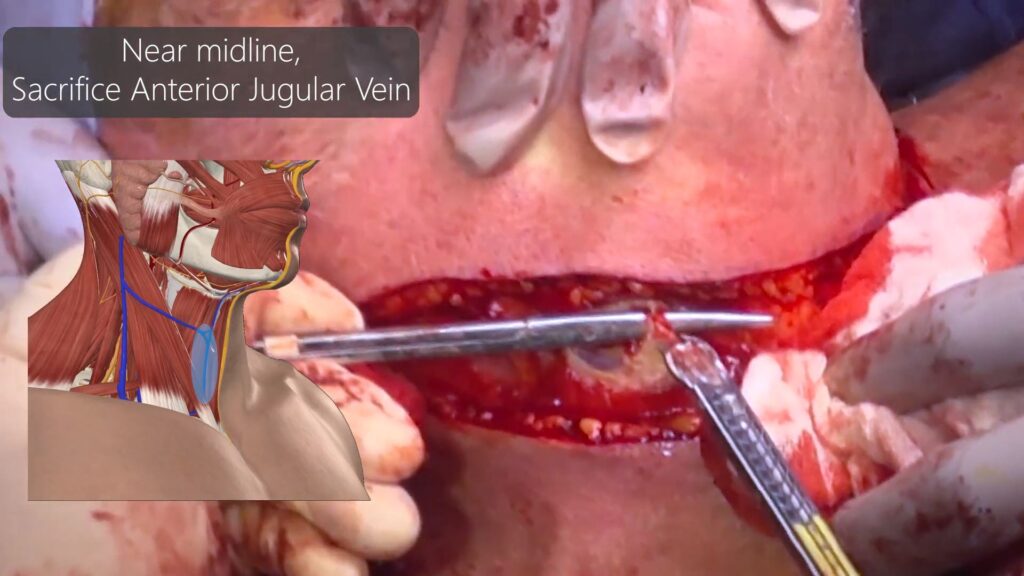
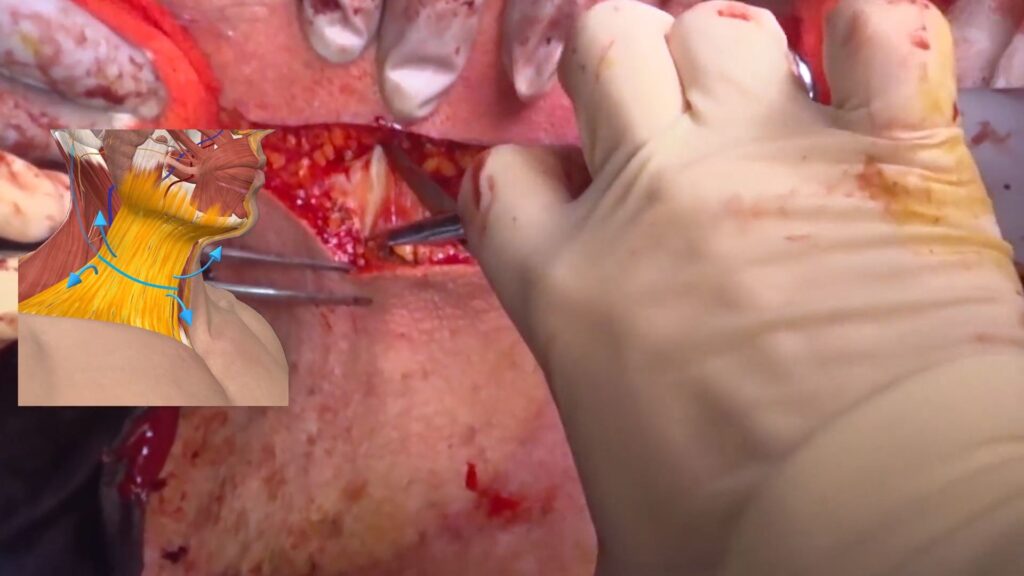
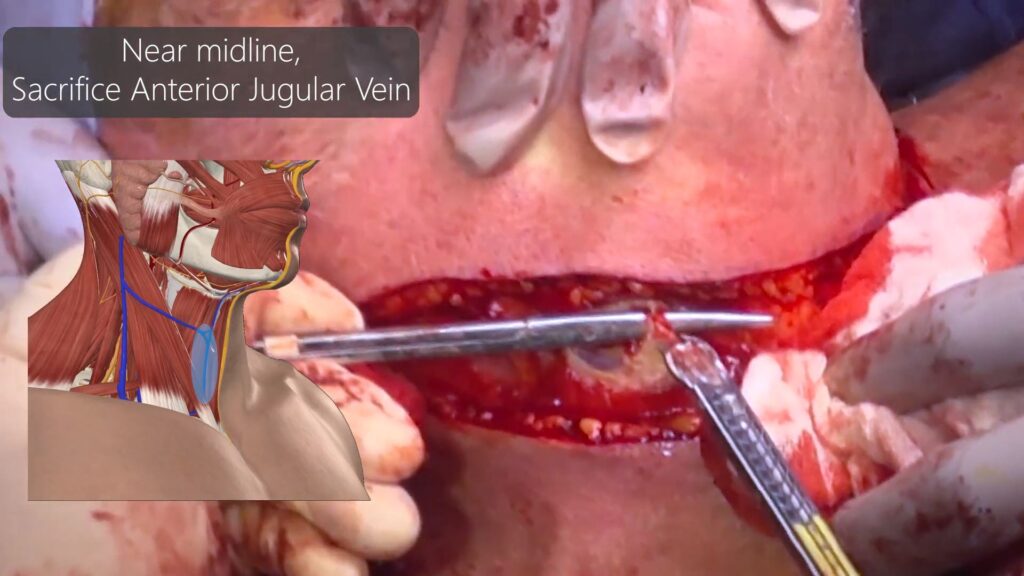
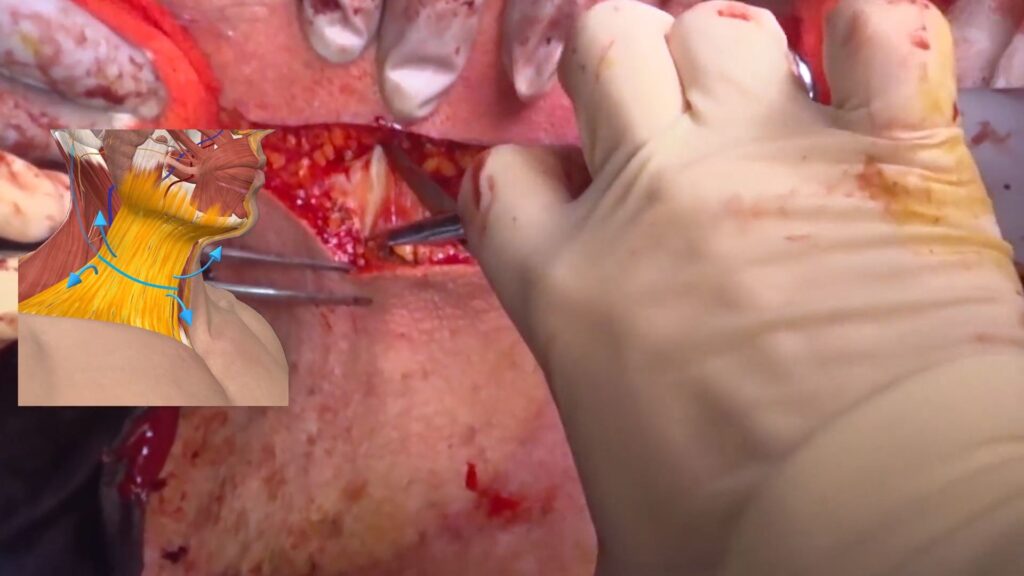
Subplatysmal Structures
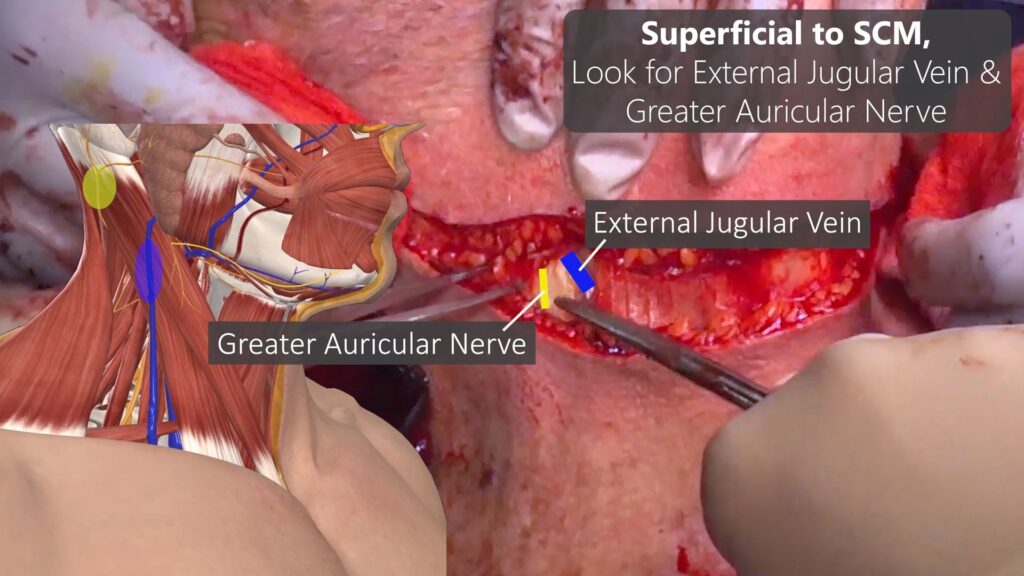
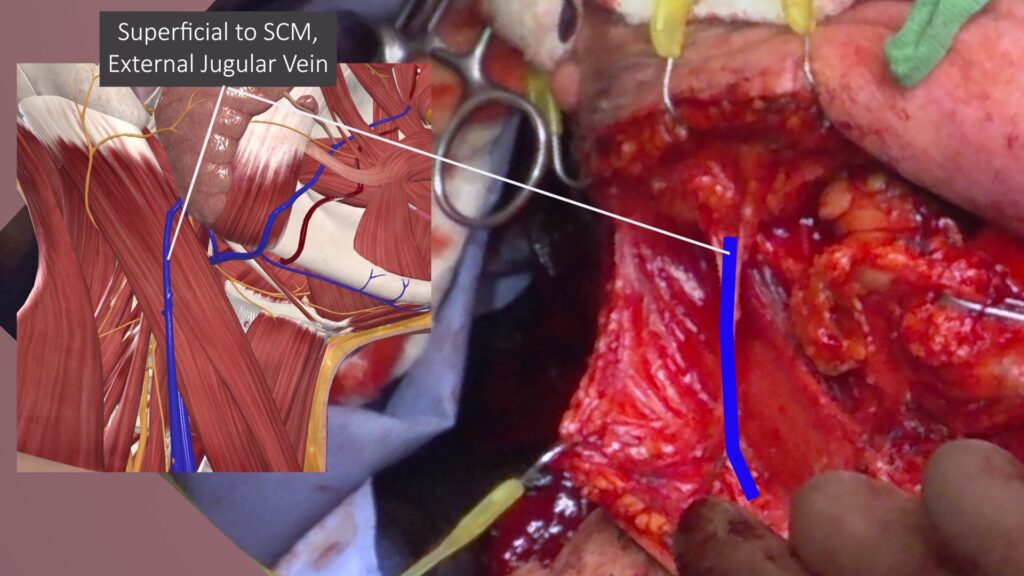 ‘
‘
Level 1A
Level 1B Dissection
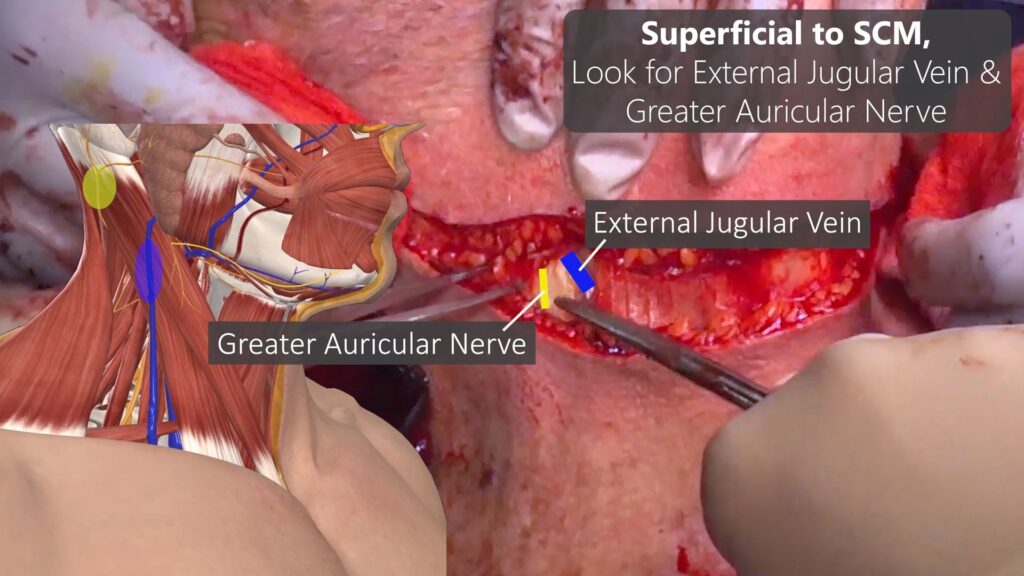
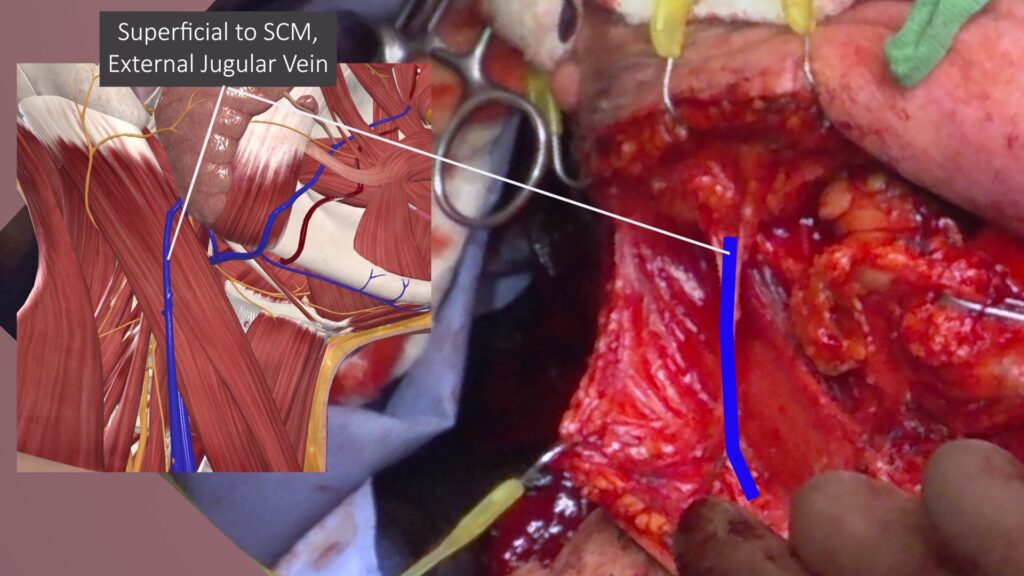
Level 2-4 Neck Dissection
Great vessels and Nerves located deep to Digastric & Omohyoid Muscles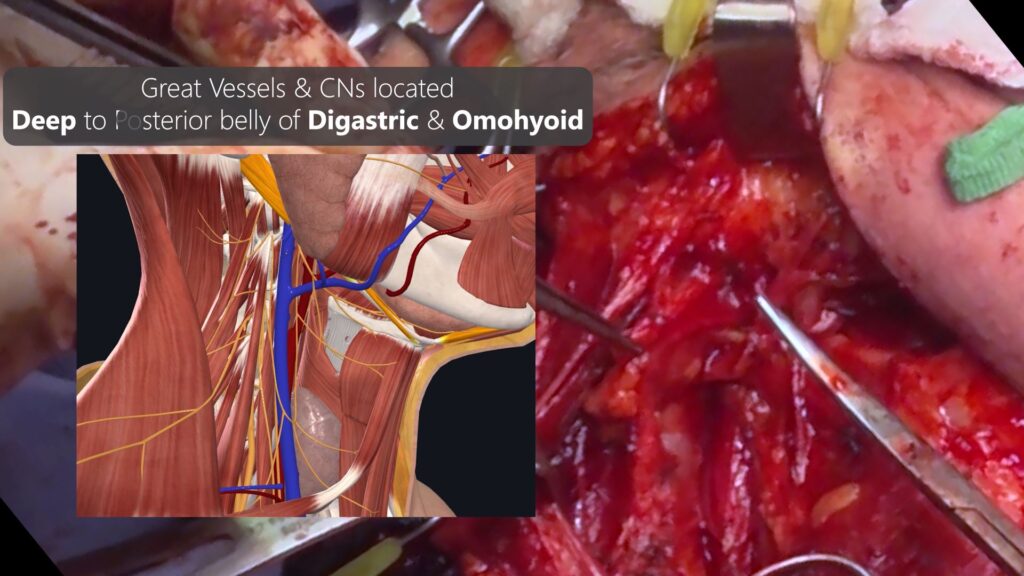
Between IJV and Carotid Artery, Vagus Nerve is Located. Unless you are doing Thyroid or Spine surgery, Avoid dissecting Medial to Carotid.
RLN and Sympathetic Chain located medial to Carotid Artery.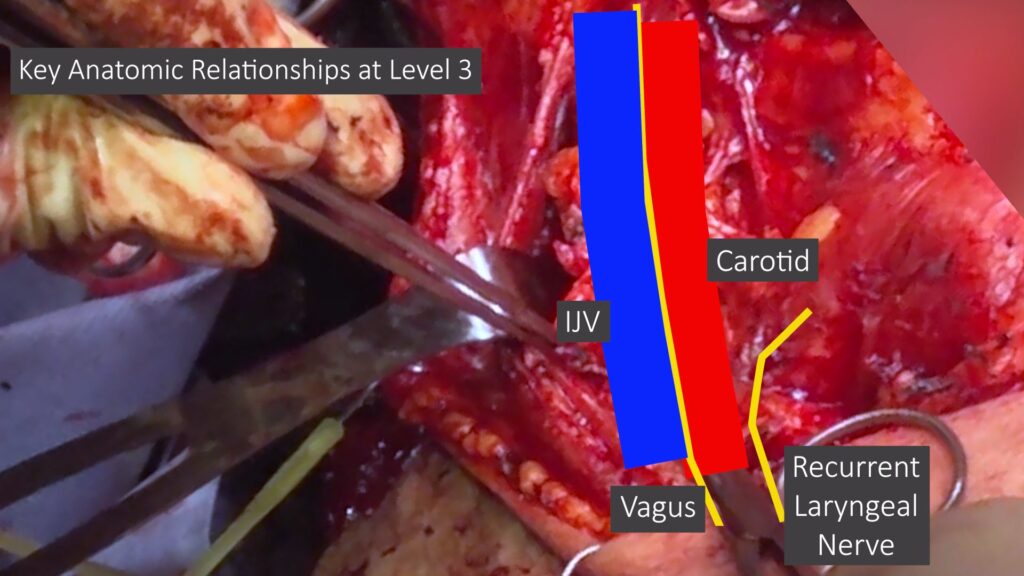
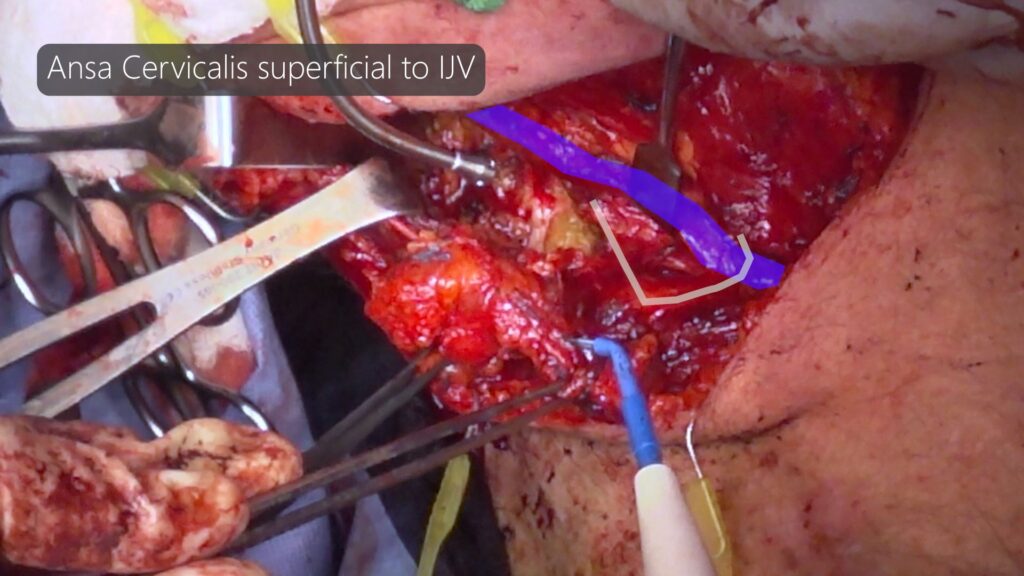
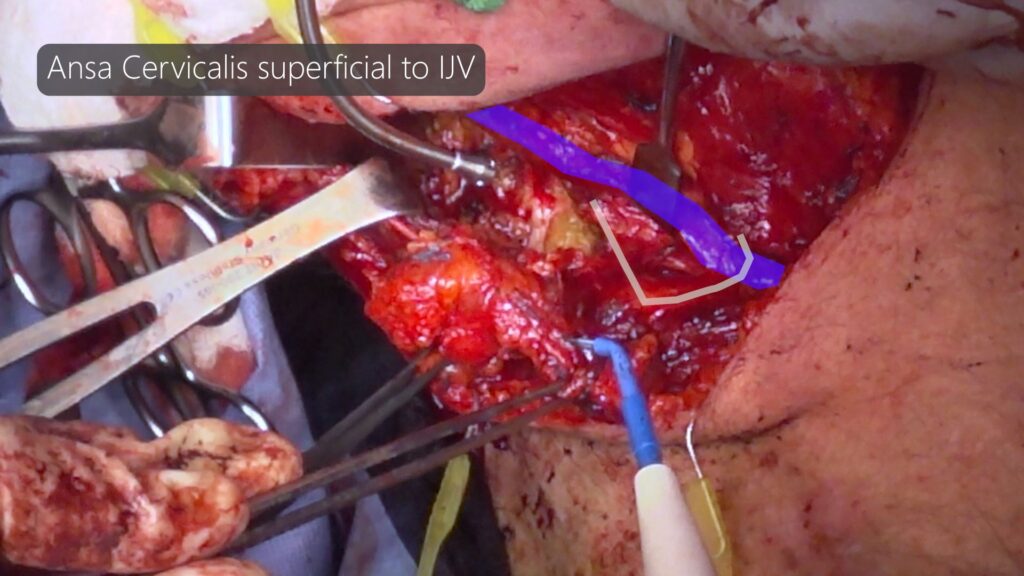
Ansa Cervicalis is located superficial to IJV. Aside from CN11 at level 2, no other nerves do that in Level 3.
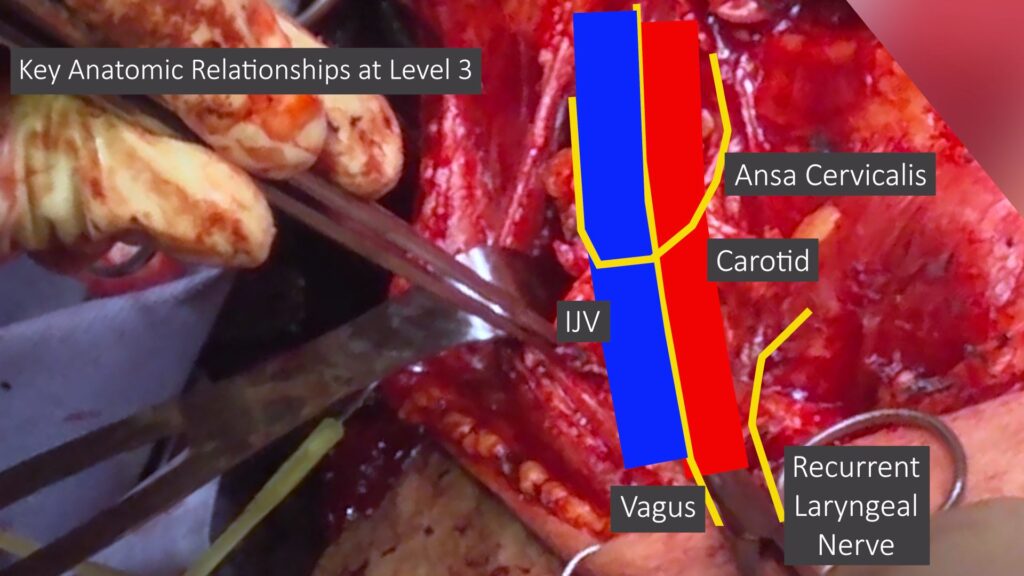
Ansa cervicalis can lead you to CN 12 (Hypoglossal nerve) in level 2
Key Level 2 Relationships
Be aware of variation where IJV being lateral to CN11. Otherwise, you may cut the IJV by accident.
If IJV transected by accident beyond repair, you can sacrifice the IJV without consequence as long as opposite IJV preserved.
If bilateral IJV sacrificed, patient will likely suffer sustained venous congestion that does compensate with time but it will result in impressive head swelling.
If you have hard time telling difference between small nerve and vessels…
At Level 2 dissection along superior aspect (near mandible), use 3 retractors to get proper exposure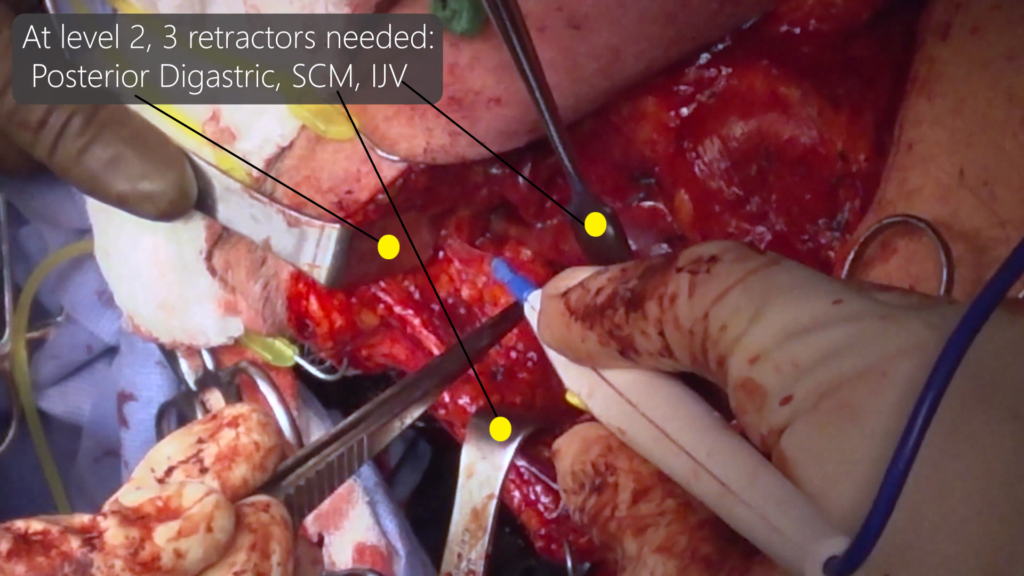
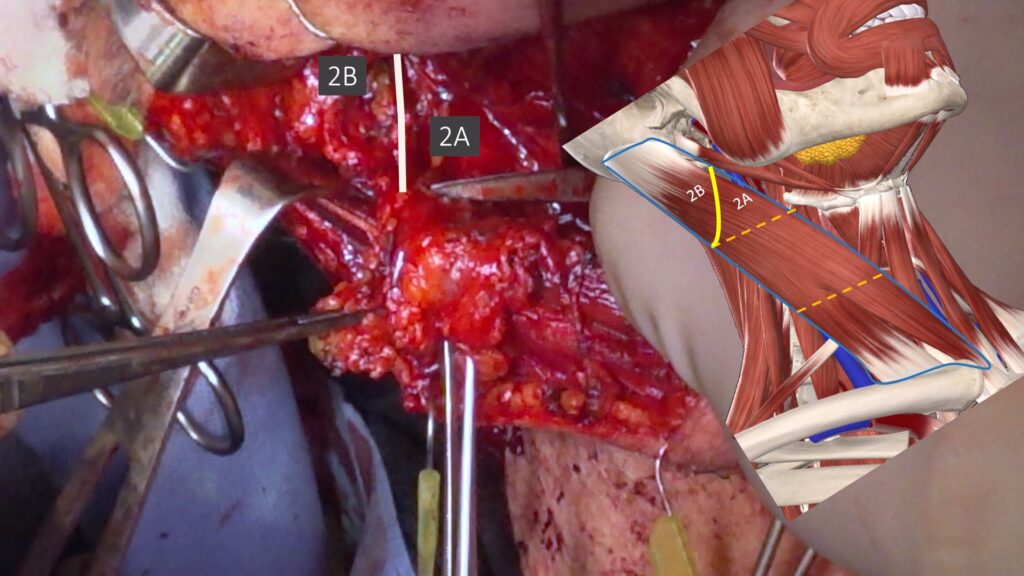
Level 2A and 2B are separated by CN11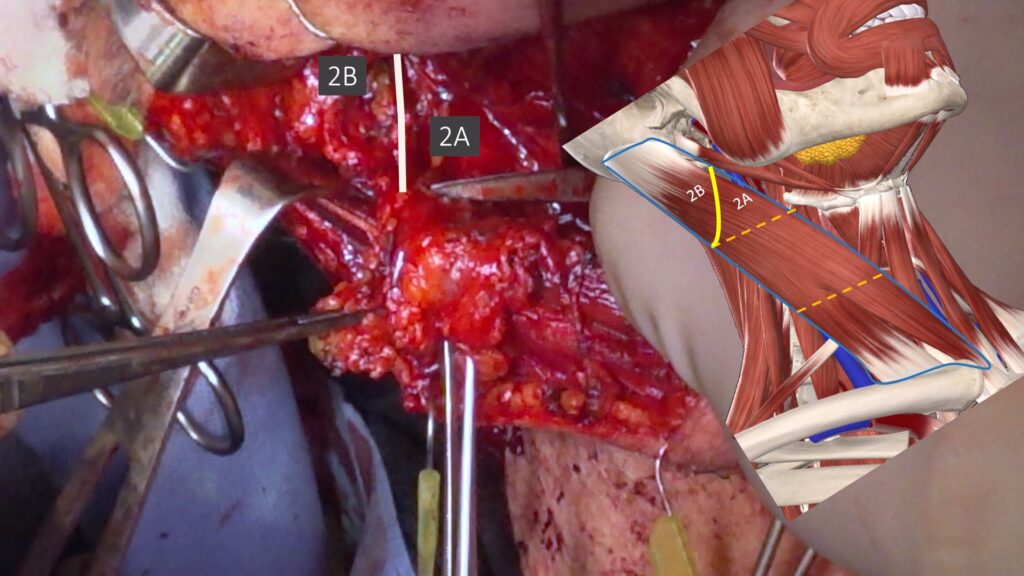
Deep tissue plane for Level 2-4 (except medial aspect of Level 4)
At Level 4, be mindful of deep tissue plane should be superficial to phrenic nerve.
If you hug the prevertebral fascia, you may cut the nerve.
Phrenic Nerve is located superficial to anterior scalene muscle.
Brachial Plexus is located between anterior & middle scalene muscles. If you are seeing muscle fibers, you are dangerously too deep!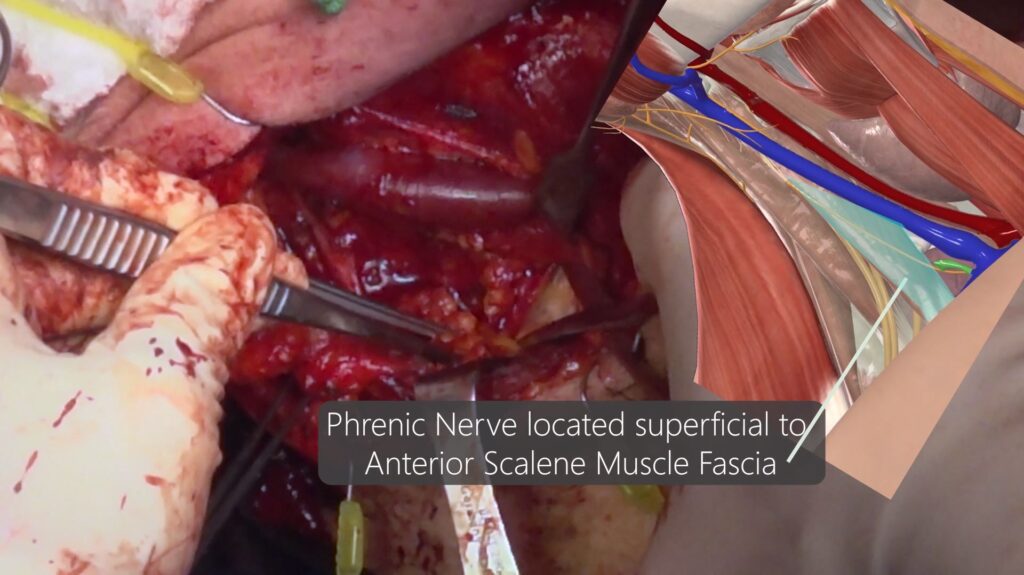

 ‘
‘