Comprehensive Guide to Level 1-4 Neck Dissection Techniques for Beginning Surgeons
Author: Dr. Thomas Lee, MD, FACS
Abstract
Neck dissection is a critical surgical procedure utilized in the management of head and neck malignancies. Understanding the anatomical layers and their relationships is crucial for minimizing complications and optimizing outcomes. This educational article outlines step-by-step techniques for performing level 1 through level 4 neck dissection safely, emphasizing the preservation of vital structures.
Introduction
Neck dissection entails the surgical removal of lymphatic tissue from cervical lymph node regions. It is vital for trainees to understand that the procedure’s sequence may vary among surgeons and specific clinical scenarios. This guide aims to provide a foundational approach for beginning surgeons.
Anatomical Considerations
Overview of Layers
- Superficial Layer: Skin and subcutaneous tissue.
- Platysma Muscle: The first major muscle layer encountered. Leave the platysma attached to the skin flap.
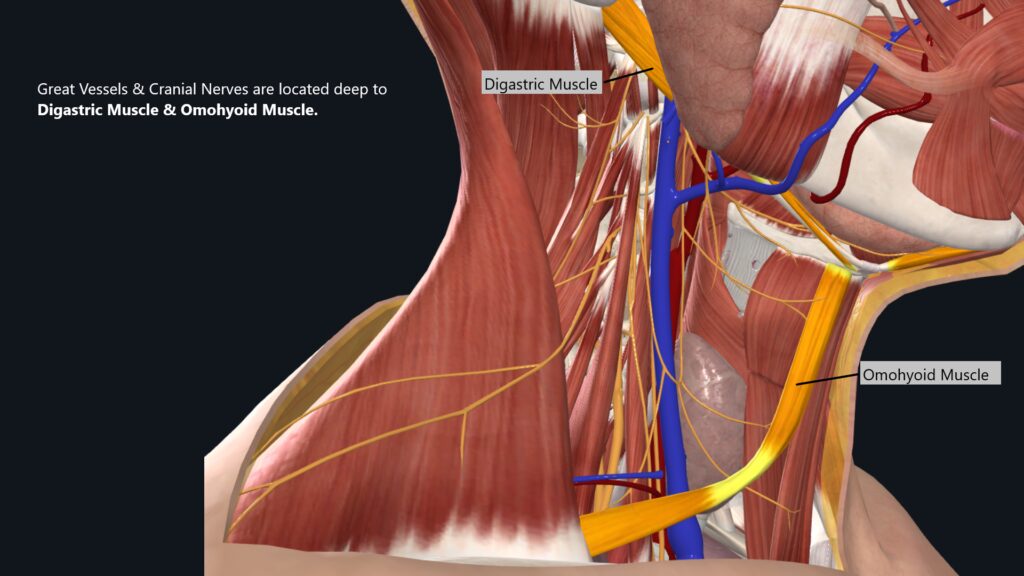
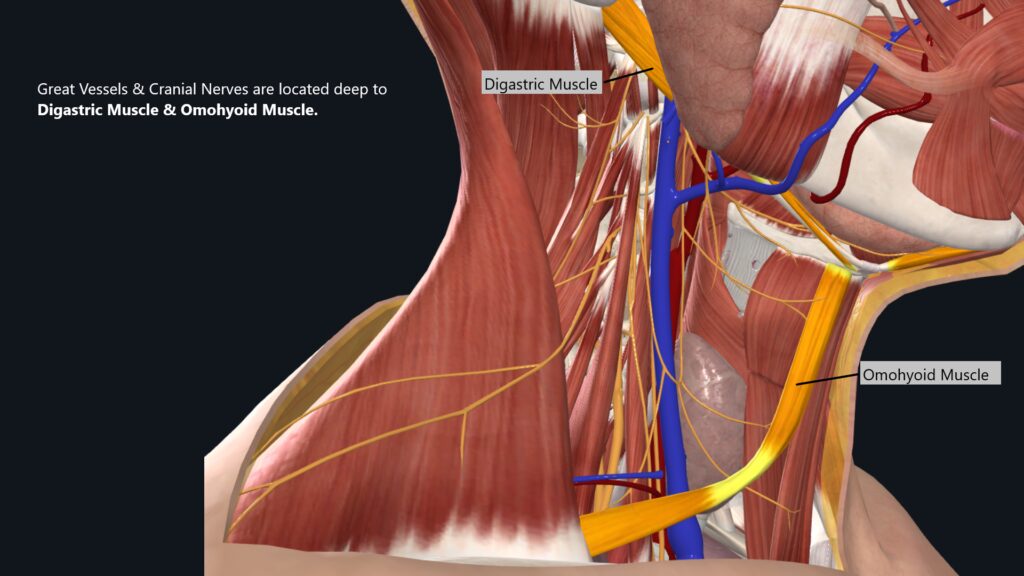
- Deep Structures: Including major vessels and nerves. Key critical structures that need to be preserved will be located deep to digastric & omohyoid muscles.
Key Structures to Preserve (Assuming no issues with cancer margins)
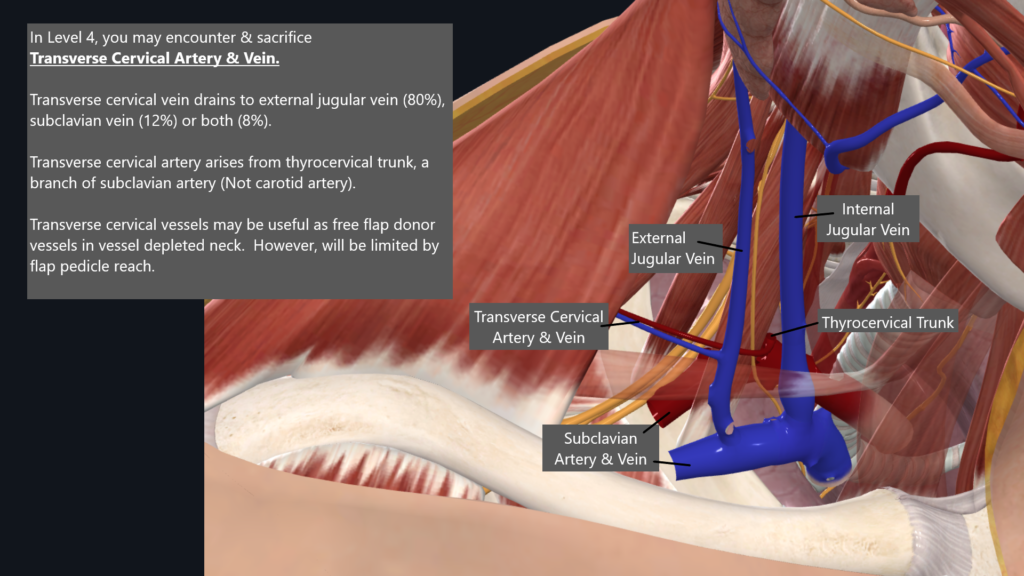
- External Jugular Vein = Potential Flap Donor Vessel
- Marginal Mandibular Nerve = Lower Lip Movement
- Greater Auricular Nerve = Routinely sacrificed in traditional neck dissection. Saved in face/neck lift. Sensory input to ear lobe.
- Accessory Nerve = SCM & Trapezius motor function
- Internal Jugular Vein = One IJV can be safely sacrificed without any noticeable consequence. However, if bilateral IJV sacrificed, it may lead to problematic head & neck swelling including cerebral edema. If bilateral IJV must be sacrificed, one may consider vein grafting to restore venous outflow to at least on one side. Gross bilateral IJV cancer involvement is typically considered a poor prognostic factor and the patient may be a poor surgical candidate.
- Vagus Nerve = Vocal Cords motor function, Parasympathetic innervation to internal organs. Unilateral vagus nerve sacrifice will lead to vocal cord paralysis with concerns for aspiration and dysphagia. No major internal organ derangements occur from unilateral vagus nerve sacrifice.
- Phrenic Nerve = Diaphragm motor function
- Brachial Plexus = Sensory, Motor & Sympathetic innervation to upper extremity
- Carotid Artery = Major blood supply to brain. Sacrifice can lead to hemi-stroke. Gross tumor involvement of carotid artery is traditionally assumed to be unresectable.
Principles of Neck Dissection: Balancing Tumor Control with Functional Preservation
The primary objective of neck dissection is to eradicate all tissues that may harbor malignant cells, thereby achieving optimal oncologic control. However, this goal must be balanced with the preservation of vital structures and minimizing functional deficits.
General Principles:
- Targeted Resection: The ideal scenario involves removing only those structures demonstrably involved or in close proximity to the tumor.
- Marginal Control: In cases of gross tumor invasion, structures may be sacrificed to obtain wider margins and ensure complete tumor removal.
- Carotid Artery Preservation: Traditionally, carotid artery involvement (T4b) is considered unresectable due to the high risk of complications. There is a significant risk of hemi-stroke from carotid artery sacrifice unless preoperative balloon occlusion study has been performed to ensure adequate collateral flow exists from the opposite side.
- Spine Involvement: Gross tumor involvement of the spine is similarly also considered unresectable due to the limited potential for survival improvement with surgical intervention.
Structures Commonly Preserved:
- Internal Jugular Vein (IJV)
- External Jugular Vein (EJV)
- Spinal Accessory Nerve (CN XI)
- Hypoglossal Nerve (CN XII)
- Vagus Nerve
- Phrenic Nerve
- Brachial Plexus
- Carotid Artery
Functional Compromise:
- Extensive Resection: In rare circumstances, resection of all structures except the carotid artery may be considered. However, this incurs significant functional deficits depending on the structures sacrificed and necessitates extensive pre-operative counseling.
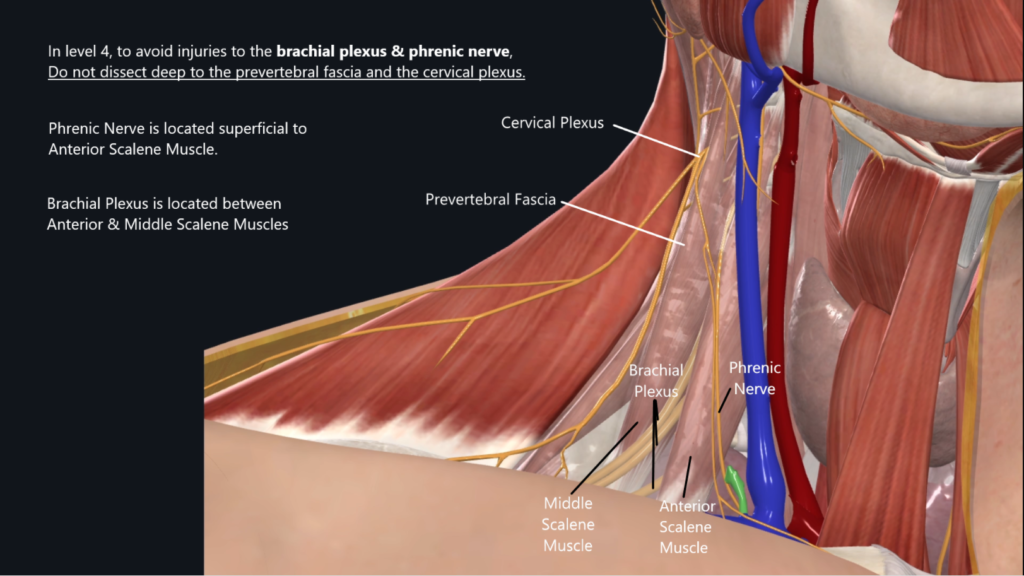
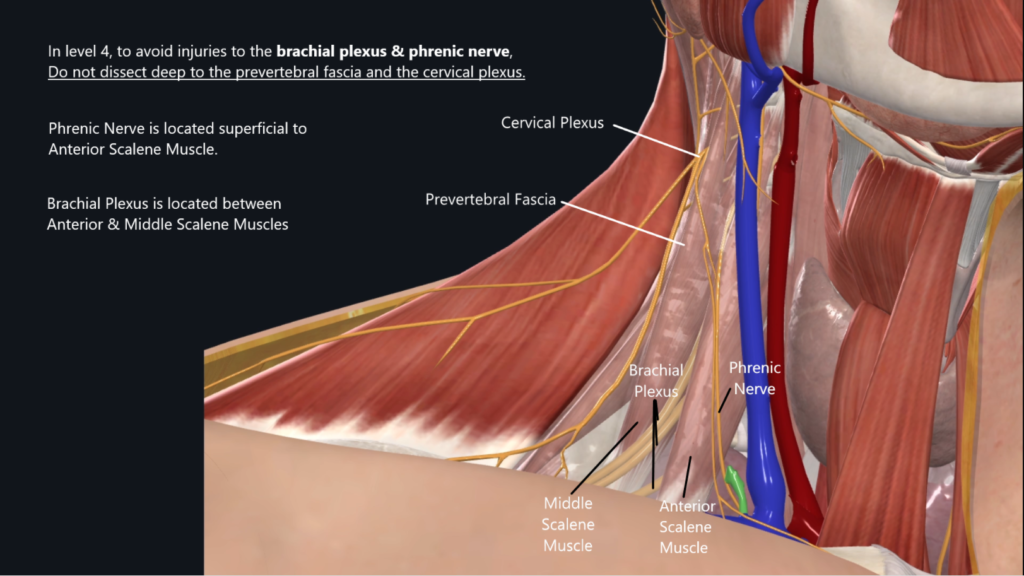
- Brachial Plexus Injury: Brachial plexus injury is a devastating injury that should never occur in routine neck dissection. It can occur from dissecting too deep in level 4 neck dissection. Intentional resection of the brachial plexus is essentially non-existent in traditional head and neck cancer neck dissections. It is reserved for cases with direct tumor invasion of brachial plexus with significant pre-operative upper extremity compromise prior to surgery. Surgeons must be cognizant of close proximity of Brachial Plexus & Phrenic Nerve along the deep dissection tissue plane while performing level 4 neck dissection to avoid this devastating injury.
Neck Levels
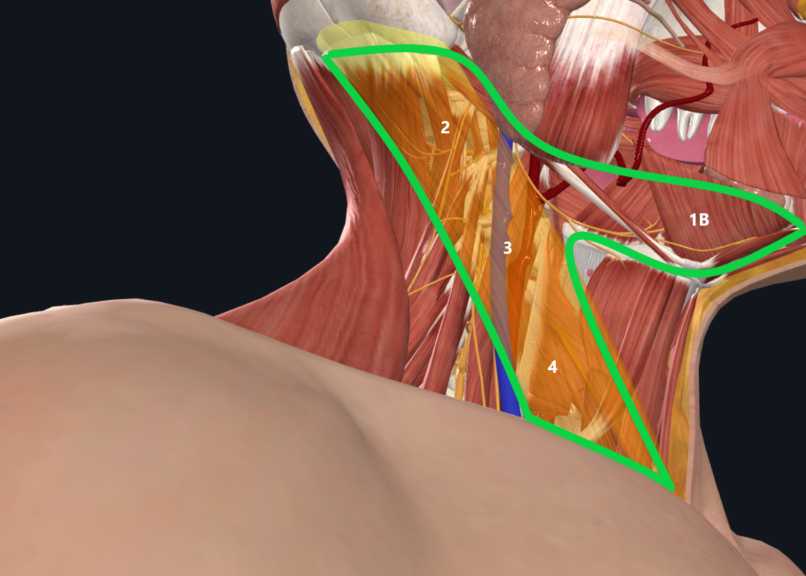
Neck dissection can be divided into different levels of the neck:
It is essential to understand that each anatomical level of the neck primarily serves to drain lymphatic fluid from specific primary tissues. This organization is crucial for both the identification of potential metastatic spread during surgical procedures and the preservation of critical structures. By comprehending the lymphatic drainage patterns associated with each level, surgeons can effectively target dissection areas while minimizing morbidity and optimizing patient outcomes.
A commonly asked question in the operating room entails the boundaries of each neck dissection level.
- Level Ia: Submental triangle
- Boundaries:
- Anterior: Midline,
- Posterior: Anterior belly of the digastric muscle
- Superior: Mandible
- Inferior: hyoid bone
- Level Ib: Submandibular triangle
- Boundaries:
- Anterior: Anterior belly of digastric muscle
- Posterior: Posterior belly of digastric muscle
- Superior: Mandible
- Inferior: Hyoid
- Level II: Upper jugular nodes
- Boundaries:
- Anterior: border of the stylohyoid muscle
- Posterior: posterior border of the sternocleidomastoid muscle
- Superior: skull base
- Inferior: Level of the hyoid bone (clinical), carotid bifurcation (surgical)
- *Level II is divided by the accessory nerve into levels IIa (anteriorly) and IIB (posteriorly).
- Level III: Middle jugular nodes
- Boundaries:
- Anterior: lateral border of the sternohyoid muscle.
- Posterior: posterior border of the sternocleidomastoid muscle
- Superior: hyoid bone
- Inferior: cricoid notch (clinical), omohyoid muscle (surgical)
- Level IV: Lower jugular nodes
- Boundaries:
- Anterior: lateral border of the sternohyoid muscle.
- Posterior: posterior border of the sternocleidomastoid muscle
- Superior: cricoid notch (clinical), omohyoid muscle (surgical)
- Inferior: clavicle
- Level V: Posterior triangle
- Boundaries:
- Anterior: posterior border of the sternocleidomastoid muscle
- Posterior: anterior border of the trapezius muscle
- Inferior: clavicle
- Level V was subdivided into level VA (superiorly) and VB (inferiorly)
- Levels VA and VB are separated by a horizontal plane marking the inferior border of the anterior cricoid arch
- VA: spinal accessory lymph nodes
- VB: transverse cervical nodes and supraclavicular nodes (with exception of the Virchow node, in level IV)
- Level VI: Nodes of the anterior compartment – pretracheal, paratracheal, precricoid lymph nodes
- Boundaries:
- Lateral: lateral border of the sternohyoid muscle
- Superior: hyoid bone
- Inferior: suprasternal notch
Neck Dissection Technique
Preoperative Preparations
- Patient Positioning: Ensure proper positioning with the neck extended.
- Incision Planning: Mark all incision lines based on the extent of disease and planned dissection.
- No long term paralytic anesthetic agent used during neck dissection to detect motor nerves: in surgical cases where motor nerves are to be identified (such as in neck dissection), I ask no long-term paralytic agents are utilized during the case so that we can detect muscle movements when motor nerves are stimulated.
Incisional Technique
- Curved Incision from Mastoid: Make a gentle curve towards the level of the cricoid cartilage or lower than the cricoid. Avoid making the incision high towards the hyoid to facilitate easier closure post-dissection.
- Bilateral Dissection: If a bilateral neck dissection is required, design a wide apron incision to ensure adequate skin flap mobility.
Dissection Procedures
Subplatysmal & Superficial to SCM
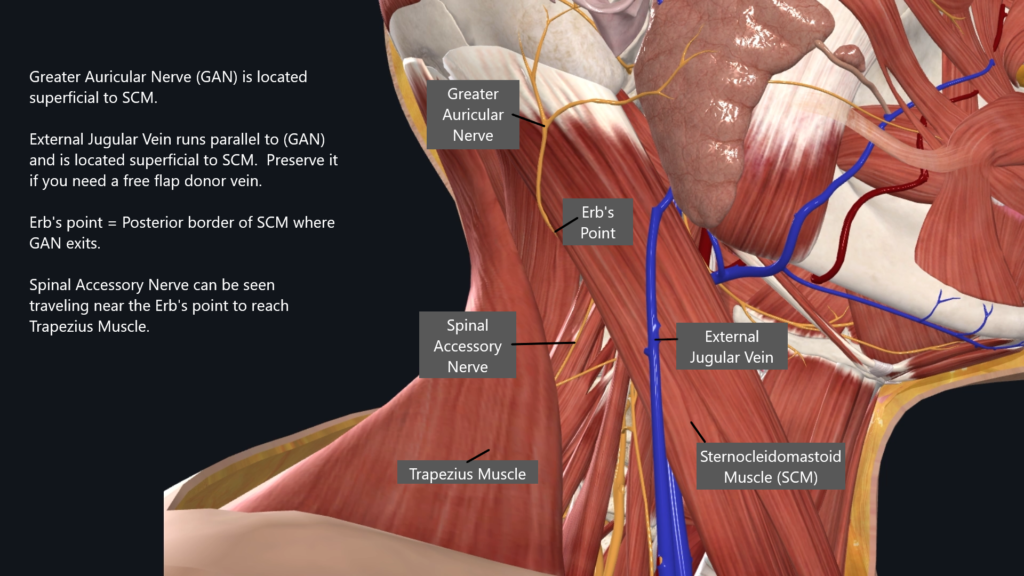
- Identify and Protect Structures: During dissection, identify the external jugular vein and marginal mandibular nerve while carefully reflecting the skin flap.
- Leave EJV down on the SCM.
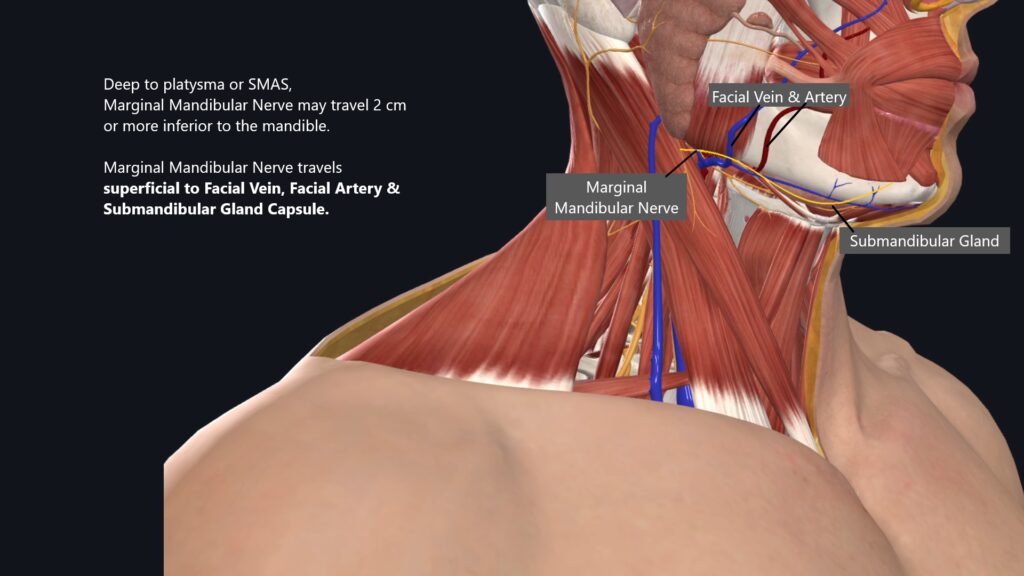
- Along the superior border of the neck dissection, look for marginal mandibular nerve as you are dissecting in the subplatysmal tissue plane. Once the marginal mandibular nerve is identified, reflect it superiorly along with the neck skin flap to gain access to the content deep to the marginal mandibular nerve.
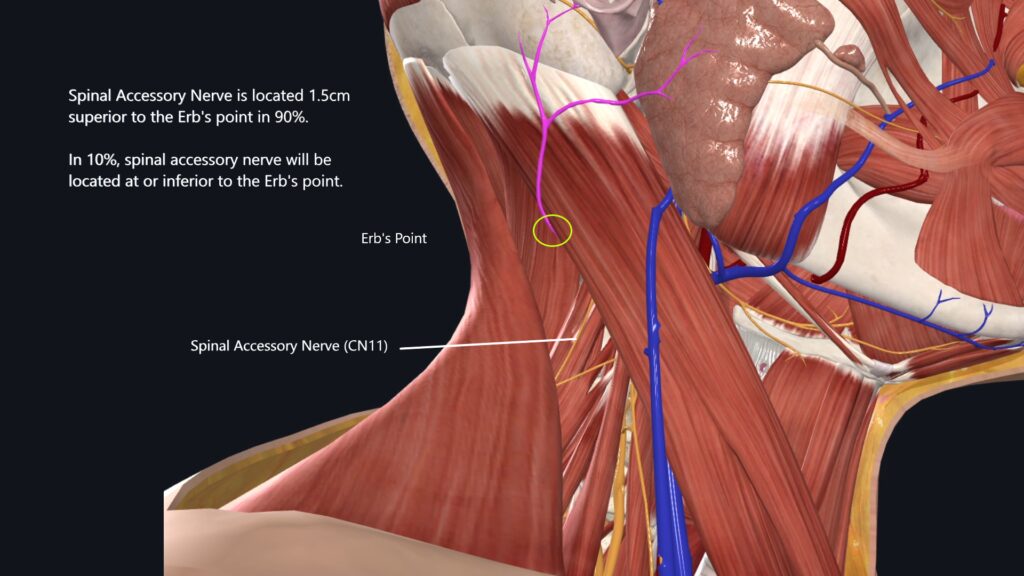
- Great auricular nerve runs parallel to the external jugular vein. Erb’s point is at the posterior border of SCM where the greater auricular nerve exists and runs superficial to SCM. Spinal accessory nerve (CN11) can be identified near Erb’s point as it travels towards the trapezius muscle.
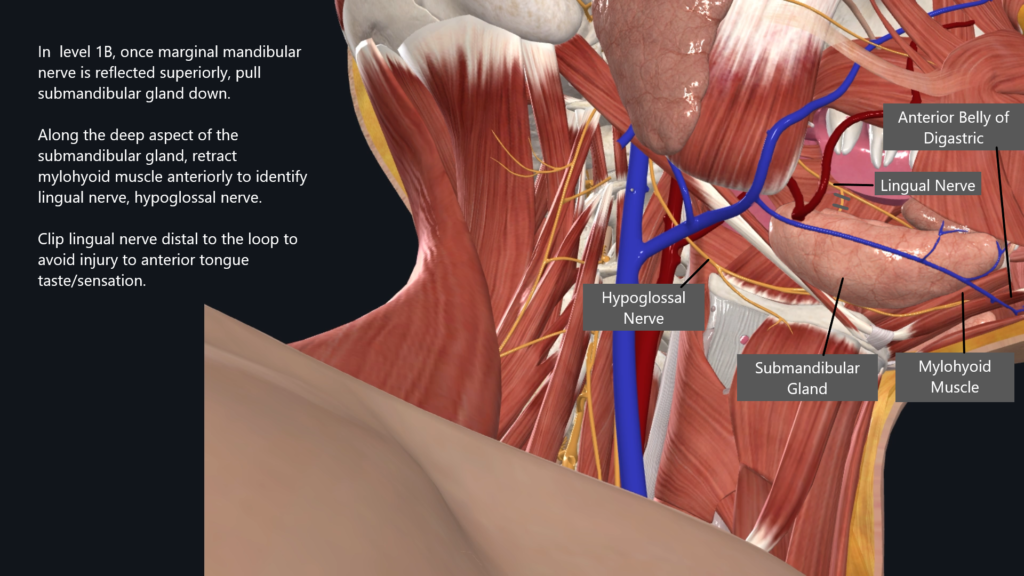
Level 1B Dissection
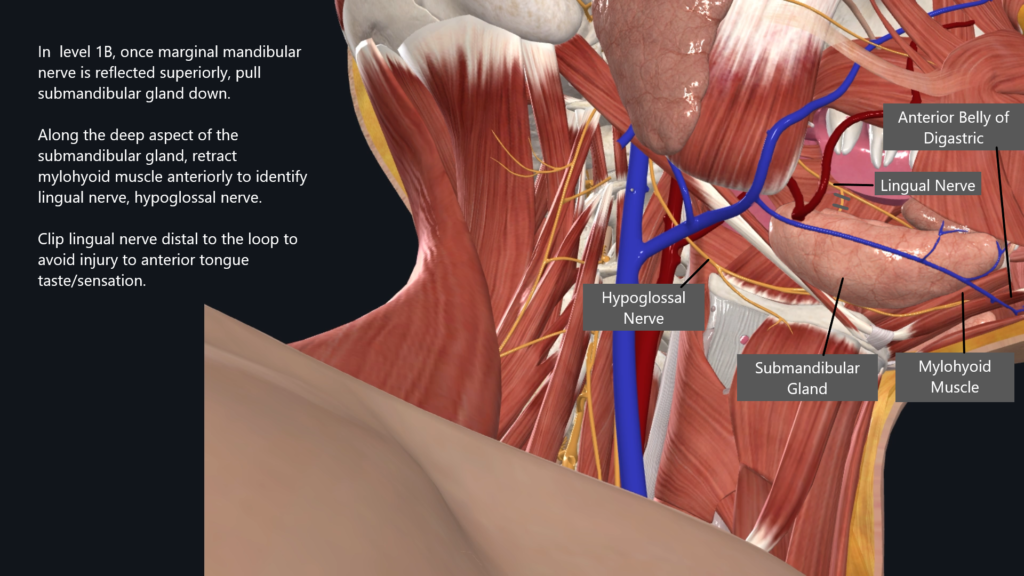
- Focus on Submandibular Gland:
- Reflect the marginal mandibular nerve superiorly.
- Expose the deep aspect of the submandibular gland. The gland is typically dissected along its superior aspect when dissecting along the superficial aspect of the gland. The gland is then dropped inferiorly once the marginal mandibular nerve is reflected.
- Identify Nerves:
- Along the deep aspect of the gland, identify two nerves:
- Hypoglossal Nerve: Critical for tongue mobility; preserve during dissection.
- Lingual Nerve: Looping down towards the submandibular gland; Disconnect the nerve away from the loop to ensure the sensory tongue innervation is intact while disconnecting it from the gland.
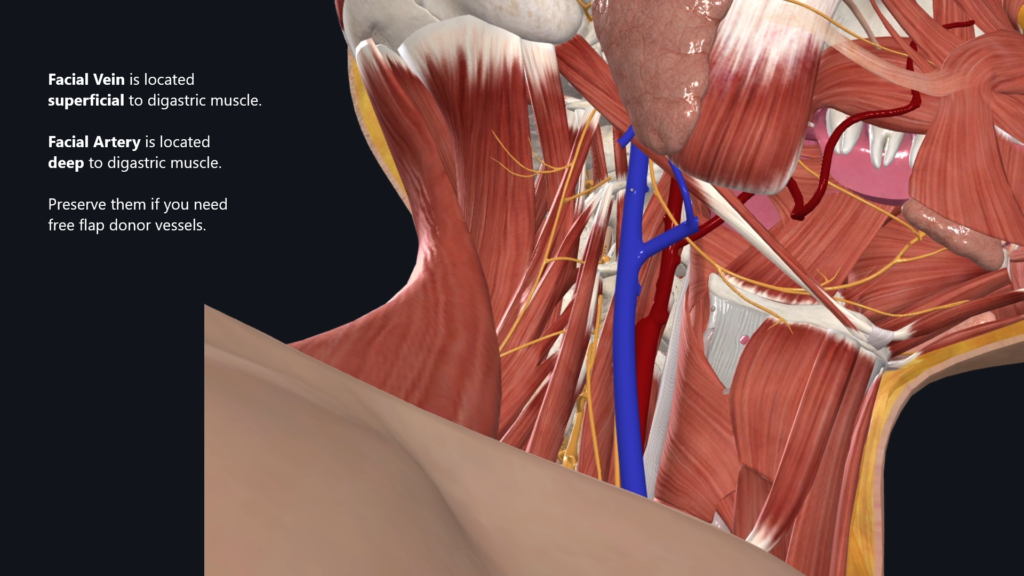
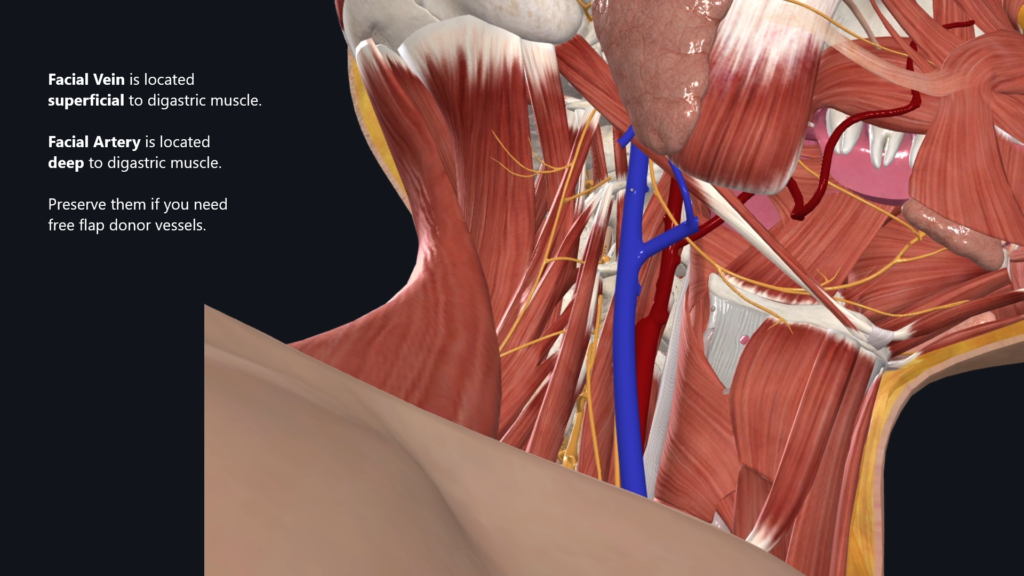
- Facial Artery and Vein: Disconnect as close to the submandibular gland capsule as possible.
- Facial Artery = Located deep to the digastric muscle
- Facial Vein = Located superficial to digastric muscle
Level 1B Subplatysmal Structures
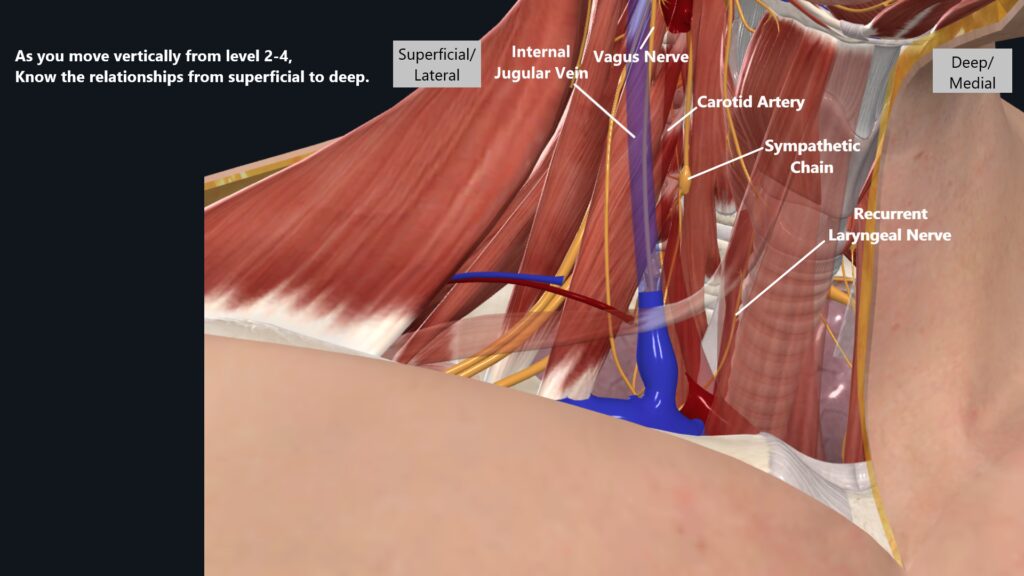
Level 2-4 Structures
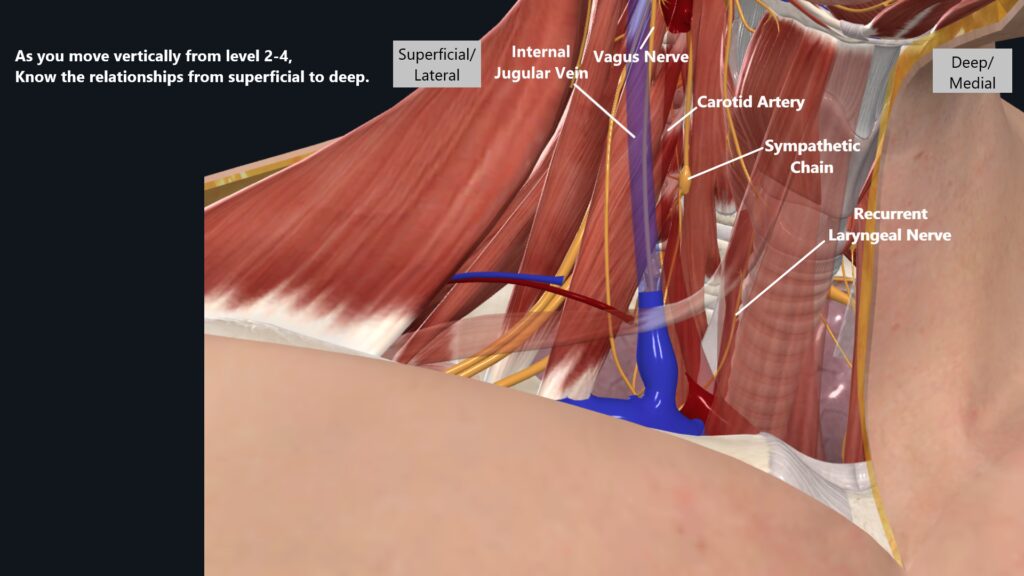
- Locate Internal Jugular Vein: Start your dissection deep to the sternocleidomastoid and digastric muscles. Once IJV is identified, you can move vertically between level 2 to 4 by following IJV.
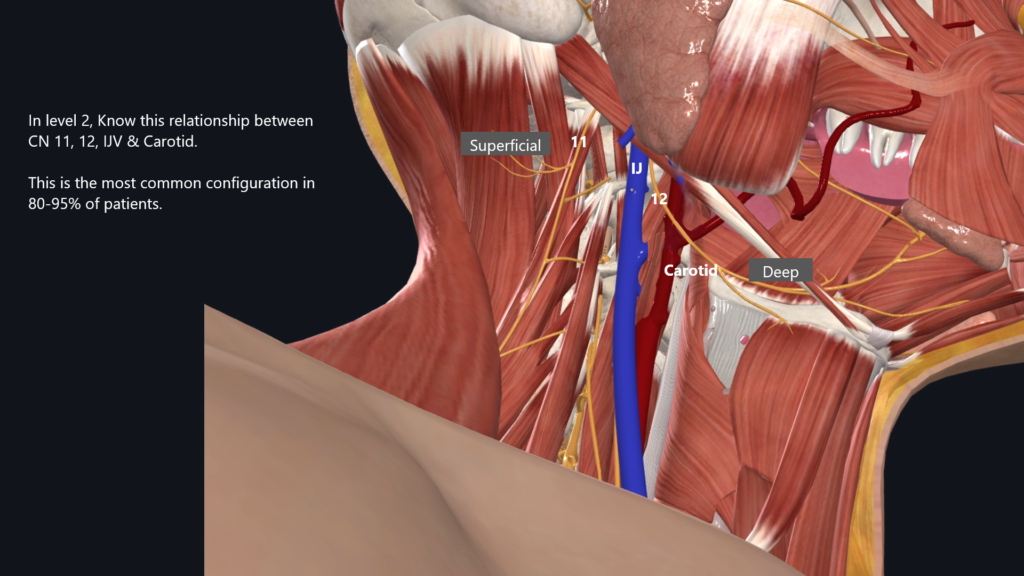
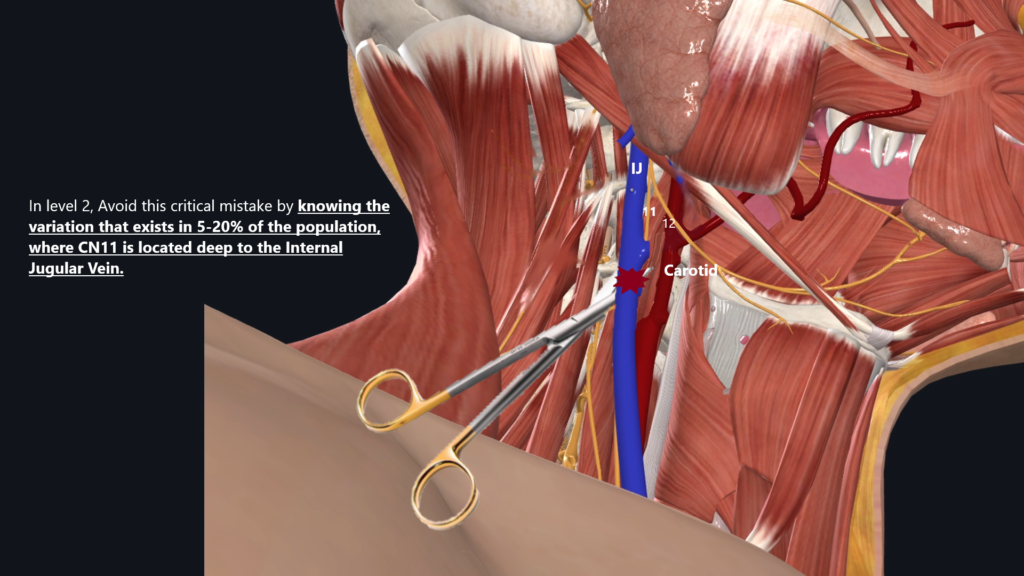
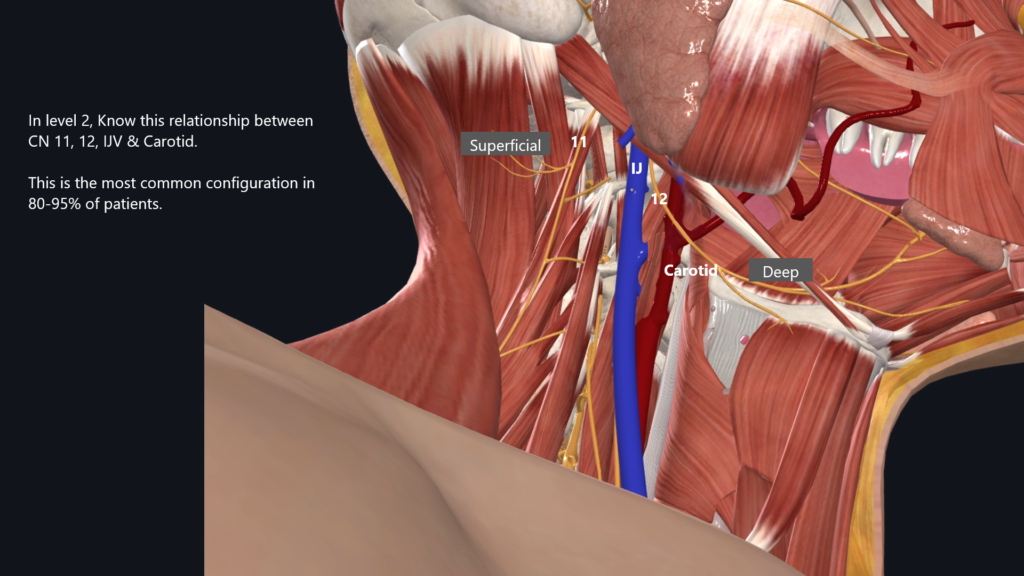
- Identify Cranial Nerve Relationships at Level 2:
- Note the arrangement from superficial to deep: Accessory Nerve -> Internal Jugular Vein -> Hypoglossal Nerve -> Carotid Artery.
- Preserve Essential Nerves:
- CN 12 = hypoglossal nerve is located between the IJV and Carotid artery. This provides tongue motor function and should be preserved unless gross tumor involvement is detected intraoperatively
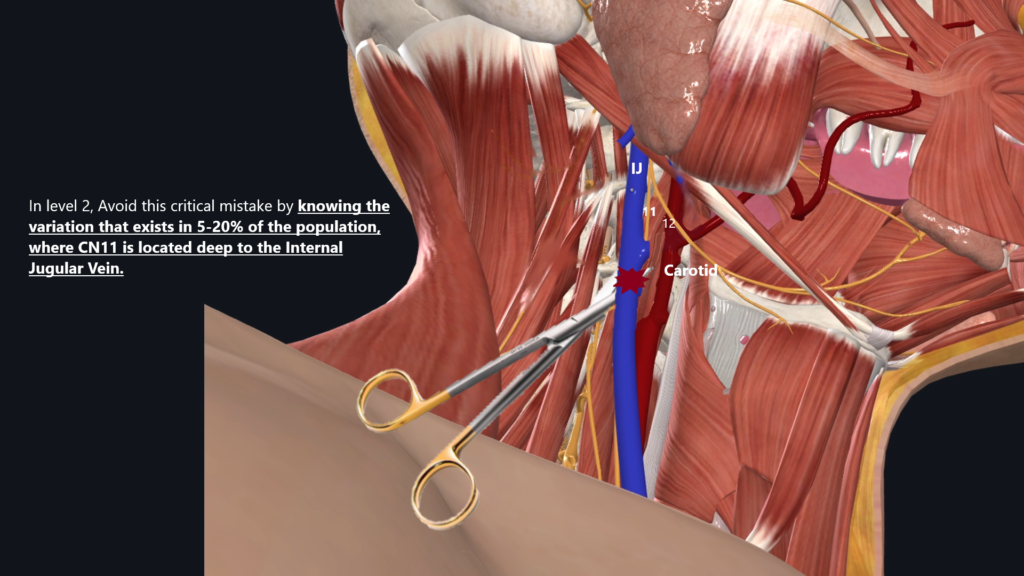
- CN 11 = accessory nerve is located usually superficial to IJV. However, there can be an anatomic variation where the CN11 is located deep to IJV. This is important to recognize so that you do not accidentally cut through IJV.
- Vagus Nerve = Runs vertically between the carotid artery & internal jugular vein
- Ansa Cervicalis = Emerges from hypoglossal nerve. Located superficial to IJV. Provides motor function to strap muscles. Ansa Cervicalis is typically sacrificed without major issues although it does provide motor function to strap muscles.
- Sympathetic Chain = Not typically seen during routine neck dissection. Located medial to carotid artery near the spine. If sacrificed, will result in Horner syndrome.
Key Level 2 Anatomic Relationship
Level 2 -4 Structures
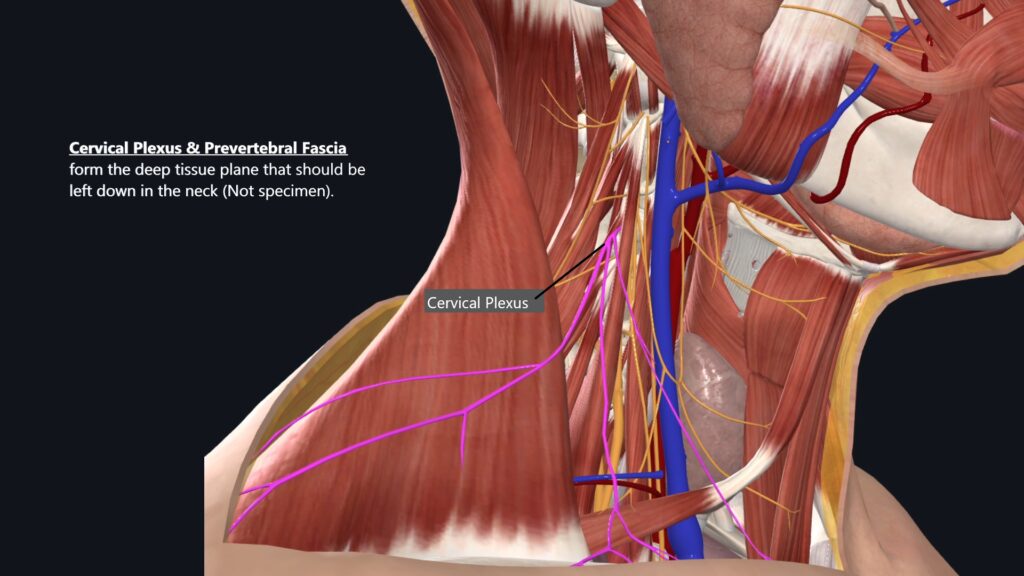
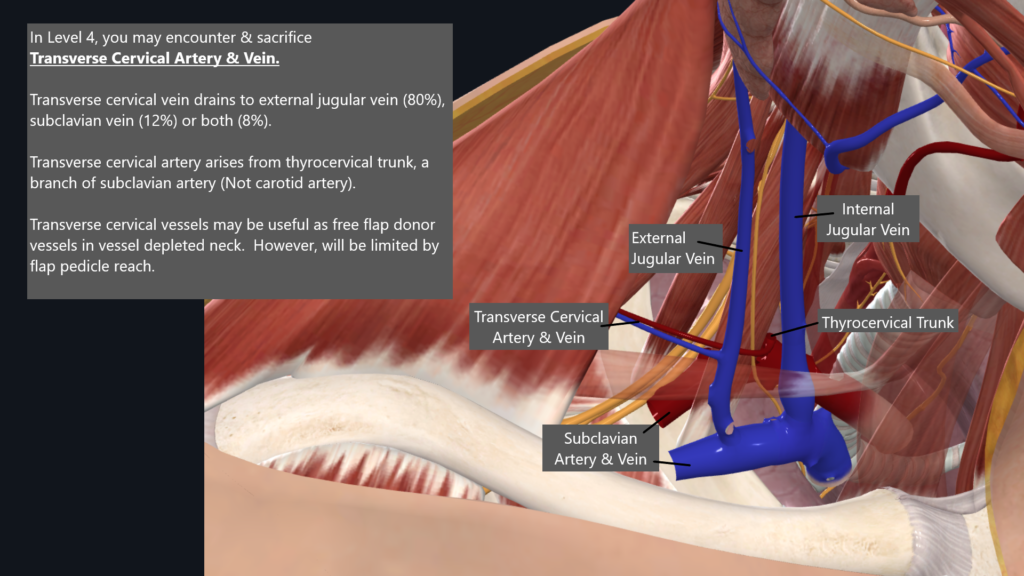
Level 4 Dissection
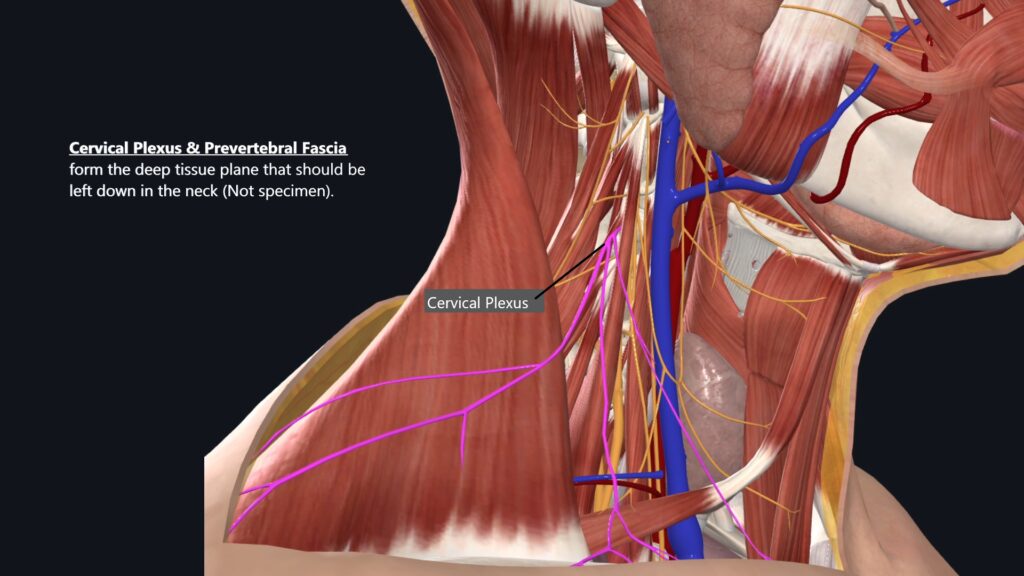
- Identify Prevertebral Fascia: Surrounds the neck muscles and cervical plexus. Do not dissect deeper than this structure to protect brachial plexus & phrenic nerve. Typically, sensory nerve rootlets also serve as deep tissue plane boundary along with prevertebral fascia.
- Avoid Injury to Critical Structures:
- Phrenic Nerve: Located superficial to the anterior scalene muscle. Injury will lead to hemi-diaphragm paralysis
- Brachial Plexus: Situated between the anterior and middle scalene muscles. Injury will lead to upper extremity paralysis.
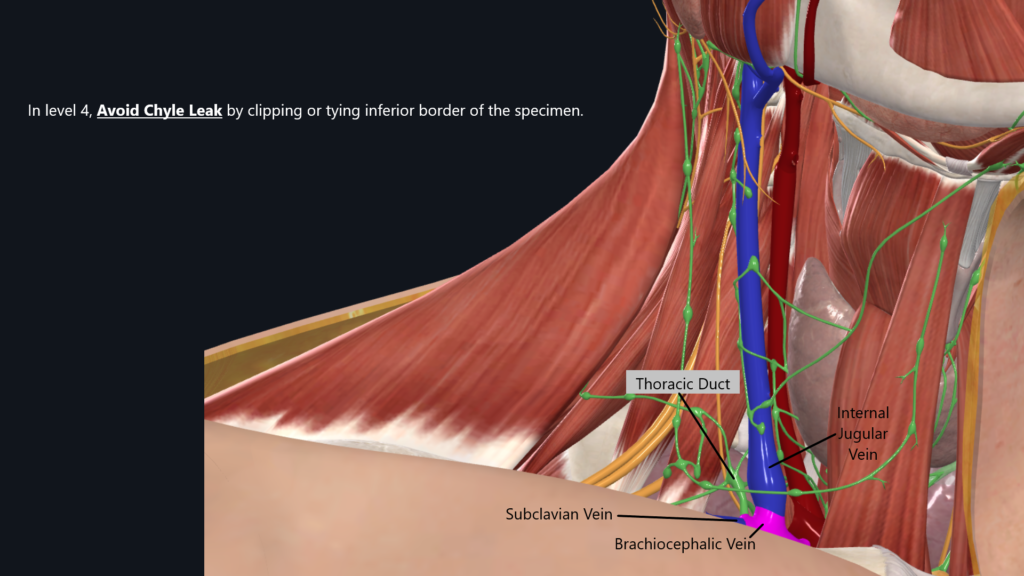
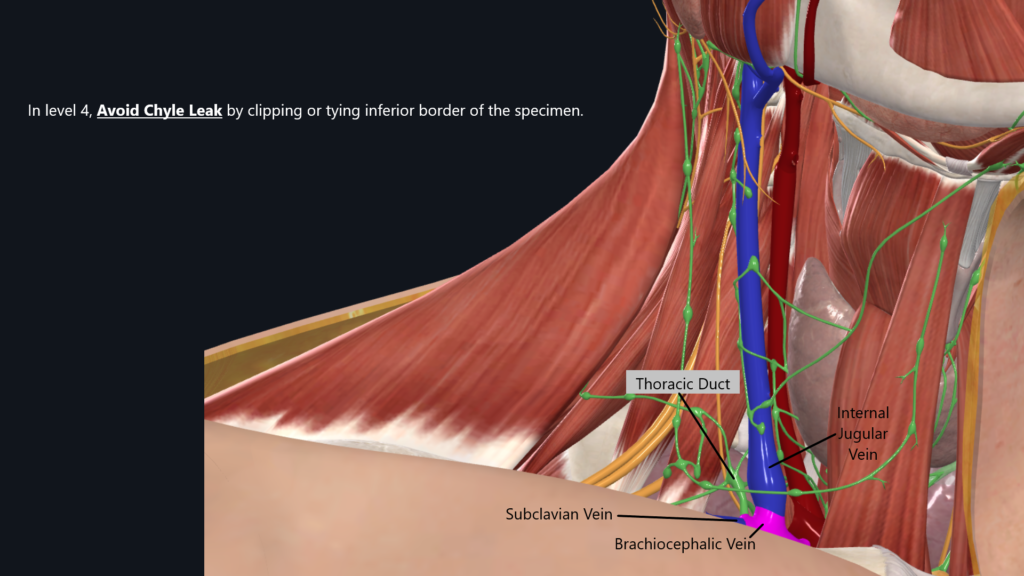
- Chylothorax Prevention:
- Be vigilant for the thoracic duct’s location during dissection; a chylothorax can occur if this structure is inadvertently injured. Consider performing the Valsalva maneuver after dissection to assess for any lymphatic leakage. You can be chyle leaks in bilateral neck, although left side is traditionally more likely where it will occur.
Conclusion
Neck dissection demands a thorough understanding of cervical anatomy and careful surgical technique to preserve vital structures. By adhering to the described techniques and considerations, beginning surgeons can navigate this complex procedure effectively. Mastery of these techniques will contribute to improved patient outcomes and enhanced surgical skills over time.